SUMMARY: Breast cancer is the most common cancer among women in the US and about 1 in 8 women (12%) will develop invasive breast cancer during their lifetime. Approximately 284,200 new cases of breast cancer will be diagnosed in 2021 and about 44,130 individuals will die of the disease, largely due to metastatic recurrence.
The HER or erbB family of receptors consist of HER1, HER2, HER3 and HER4. Approximately 15-20% of invasive breast cancers overexpress HER2/neu oncogene, which is a negative predictor of outcomes without systemic therapy. Adjuvant and neoadjuvant chemotherapy given along with anti-HER2 targeted therapy reduces the risk of disease recurrence and death, among patients with HER2-positive, early stage, as well as advanced metastatic breast cancer.
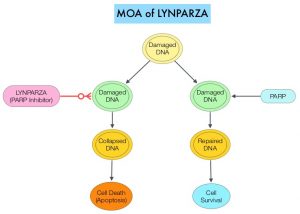
Trastuzumab is a humanized monoclonal antibody targeting HER2. It binds to the extracellular subdomain IV of the receptor and disrupts ligand independent HER2 downstream cell signaling pathways. Pertuzumab is a recombinant, humanized, monoclonal antibody that binds to the HER2 subdomain II and blocks ligand dependent HER2 heterodimerization with other HER receptors. Thus Trastuzumab along with Pertuzumab provide a more comprehensive blockade of HER2 driven signaling pathways. Dual HER2 blockade with Trastuzumab and Pertuzumab, given along with chemotherapy (with or without endocrine therapy), as first line treatment, in HER2 positive metastatic breast cancer patients, was shown to significantly improve Progression Free Survival (PFS) as well as Overall Survival (OS). The superior benefit with dual HER2 blockade has been attributed to differing mechanisms of action and synergistic interaction between HER2 targeted therapies.
Pathological Complete Response (pCR) after neoadjuvant therapy has strong prognostic significance in HER2+ breast cancer and pCR rates in HER2+/HR− tumors exceed those in HER2+/HR+ tumors, and this in turn correlates with superior Event Free Survival. The FDA approved anti-HER2 dual blockade with Pertuzumab and Trastuzumab, given along with chemotherapy for the neoadjuvant treatment of patients with HER2-positive, locally advanced, inflammatory, or early stage breast cancer, based on the NeoSphere trial, and for metastatic disease based on positive survival results in the CLEOPATRA trial. The role of chemotherapy free anti-HER2 dual blockade however has remained unclear.
ADAPT (Adjuvant Dynamic marker-Adjusted Personalized Therapy) is one of the first new generation neoadjuvant trials addressing individualization of neoadjuvant therapy in early breast cancer and was initiated to establish early predictive surrogate markers such as Ki-67 for therapy response following a short course of induction treatment, in order to maximally individualize therapy and avoid unnecessary toxicity by ineffective treatment. West German Study Group (WSG)-ADAPT trials were designed separately for HER2+/HR− and HER2+/HR+ breast cancer sub groups as they are biologically distinct, with HER2+/HR− subgroup being more aggressive but also more chemosensitive, as evidenced by response to neoadjuvant therapy and subsequent survival rates.
The WSG-ADAPT HER2+/HR- trial is a multicenter, prospective Phase II/III trial which assessed whether patients with strong early response to dual HER2 blockade alone might achieve pathological Complete Response (pCR), comparable to that of patients receiving dual HER2 blockade and chemotherapy. In this study, 134 patients (N=134) with cT1-cT4c, cN0-3 HER2+/HR- early breast cancer were randomly assigned 5:2 to either receive Trastuzumab and Pertuzumab alone in arm A or with added Paclitaxel in arm B. In Arm A, patients (N = 92) received a loading dose of Trastuzumab 8 mg/kg IV and then 6 mg/kg three weekly along with Pertuzumab 840 mg loading dose and then 420 mg 3 weekly, for a total of 12 weeks. In Arm B (N=42), in addition to Trastuzumab and Pertuzumab as administered in Arm A, Paclitaxel 80 mg/m2 IV was given every week for 12 weeks. Eligible patients had tumors that were ER and PR negative (less than 1%) and HER2-positive (IHC 2+ and FISH positive or IHC 3+ positive). After neoadjuvant treatment, surgery or histological confirmation of non-pCR by core needle biopsy within 3 weeks was mandatory. Pathological Complete Response (pCR) at surgery was defined as no invasive tumor residuals in breast and lymph nodes.
The Primary endpoint was pCR and omission of further chemotherapy was allowed in patients with pCR, and Secondary endpoints included 5 year distant Disease Free Survival (DFS) and Overall Survival (OS). An important objective of this study was to identify an early-responder population with regard to pCR after Trastuzumab and Pertuzumab alone treatment, which is strongly associated with long-term prognosis particularly in HER2+/HR− breast cancer, and assess whether this population might be spared neoadjuvant chemotherapy. Early response was defined as proliferation decrease 30% or more of Ki-67 (compared to baseline) or low cellularity (less than 500 invasive tumor cells) in the 3-week biopsy. The trial was stopped early due to the observed pCR superiority in the dual HER2 blockade plus chemotherapy group. The authors previously reported that the pCR rate in the dual HER2 blockade plus chemotherapy group was 90.5%, compared with 36.3% in the dual HER2 blockade alone. The authors have now reported the first survival data.
After a median follow-up of 5 years, there were no significant differences in DFS, distant DFS and OS between the 2 study groups. The invasive DFS rate was 98% with dual HER2 blockade and chemotherapy and 87% with dual HER2 blockade alone (HR=0.32; P=0.144). Distant DFS was 98% and 92%, respectively (HR=0.34; P=0.313) and Overall Survival was 98% and 94% (HR=0.41; P=0.422). The achievement of a pathologic Complete Response following 12 weeks of treatment was strongly associated with improved invasive DFS at 5 years, irrespective of study group (98.5% versus 82%; HR=0.14; P=0.011). The researchers also examined the benefit of neoadjuvant chemotherapy-free dual HER2 blockade alone and noted that no pCR was observed in patients with low HER2 expression (IHC 1+ or 2+ and FISH positive) and/or basal-like subtype as detected by PAM50 assay. In the total study population, low HER2 expression and/or no early response was strongly associated with worse distant DFS (P=0.029) and invasive DFS (P=0.068).
The authors concluded that excellent pCR and Survival can be accomplished in patients treated by de-escalated 12-week neoadjuvant weekly Paclitaxel and dual HER2 blockade, irrespective of additional chemotherapy use. They added that early pCR after only 12 weeks of neoadjuvant Paclitaxel plus dual HER2 blockade was strongly associated with improved outcome, and may thus serve as a predictive clinical marker for further treatment de-escalation.
De-escalated neoadjuvant pertuzumab+trastuzumab with or without paclitaxel weekly in HR-/HER2+ early breast cancer: ADAPT-HR-/HER2+ biomarker and survival results. Harbeck N, Gluz O, Christgen M, et al. J Clin Oncol 39, 2021 (suppl 15; abstr 503)