SUMMARY: Sickle Cell Disease or Sickle Cell anemia is an Autosomal Recessive disorder and affects approximately 100,000 Americans. It is estimated that it affects 1 out of every 365 African-American births and 1 out of every 16,300 Hispanic-American births. The average life expectancy for patients with Sickle Cell Disease in the United States is approximately 40-60 years. Beta thalassemia affects at least 1000 Americans and according to the WHO, more than 300,000 babies are born worldwide each year with hemoglobin disorders such as Transfusion-Dependent beta-Thalassemia (TDT) and Sickle Cell Disease (SCD). Both diseases are caused by mutations in the hemoglobin beta-globin gene.
HbSS disease or Sickle Cell anemia is the most common Sickle Cell Disease genotype and is associated with the most severe manifestations. HbSS disease is caused by a mutation substituting thymine for adenine in the sixth codon of the beta-globin chain gene. This in turn affects the hemoglobin’s ability to carry oxygen and causes it to polymerize. This results in decreased solubility thereby distorting the shape of the red blood cells, increasing their rigidity and resulting in red blood cells that are sickle shaped rather than biconcave. These sickle shaped red blood cells limit oxygen delivery to the tissues by restricting the flow in blood vessels, leading to severe pain and organ damage (Vaso-Occlusive Crises). Oxidative stress is an important contributing factor to hemoglobin polymerization with polymer formation occurring only in the deoxy state. HbS/b-0 Thalassemia (double heterozygote for HbS and b-0 Thalassemia) is clinically indistinguishable from HbSS disease. Thalassemia is an inherited hemoglobinopathy associated with an erythroid maturation defect and is characterized by ineffective erythropoiesis and impaired RBC maturation. Mutations in the hemoglobin beta-globin gene result in reduced (B+) or absent (B0) beta-globin synthesis creating an imbalance between the alpha and beta globin chains of hemoglobin, resulting in ineffective erythropoiesis. Management of Sickle Cell Disease includes pain control, transfusion support and Hydroxyurea, whereas management of beta Thalassemia include transfusion support and iron chelation therapy. None of the presently available therapies addresses the underlying cause of these diseases nor do they fully ameliorate disease manifestations. Allogeneic bone marrow transplantation can cure both these genetic disorders, but less than 20% of eligible patients have a related HLA-matched donor. There is therefore a great unmet need to find new therapies for beta-Thalassemia and Sickle Cell Disease.
Fetal hemoglobin which consists of two alpha and two gamma chains is produced in utero, but the level of gamma-globulin decreases postnatally as the production of beta-globin and adult hemoglobin which consists of two alpha and two beta chains increases. It has been noted that elevated levels of fetal hemoglobin are associated with decreased morbidity and mortality in patients with Sickle Cell Disease and Thalassemia. BCL11A gene is a repressor of gamma-globin expression and fetal hemoglobin production in adult red blood cells. Downregulating BCL11A can therefore reactivate gamma-globin expression and increase fetal hemoglobin in RBC.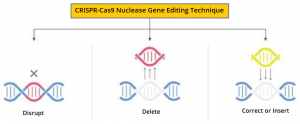
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 nuclease gene editing technique cuts the DNA at the targeted location. The authors in this study used this gene-editing technique in Hematopoietic Stem and Progenitor Cells at the erythroid-specific enhancer region of BCL11A to down-regulate BCL11A expression in erythroid-lineage cells, restore gamma-globin synthesis, and reactivate production of fetal hemoglobin.
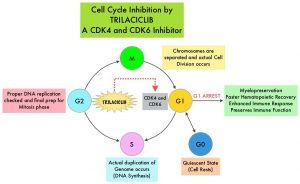
The authors reported the interim safety and efficacy data from 10 patients who received the investigational CRISPR-Cas9 nuclease gene-editing based therapy, following enrollment in CLIMB THAL-111 and CLIMB SCD-121 studies. These patients were infused with CTX001 (autologous CRISPR-Cas9-edited CD34+ Hematopoietic Stem and Progenitor Cells (HSPCs) that were genetically edited to reactivate the production of fetal hemoglobin. In the CLIMB THAL-111 and CLIMB SCD-121 open-label, PhaseI/II trials, patients with Transfusion-Dependent beta-Thalassemia and sickle cell disease , respectively, received a single intravenous infusion of CTX001. The production of CTX001 involved collection of CD34+ Hematopoietic Stem and Progenitor Cells (HSPCs) from patients by apheresis, following stem cell mobilization with either NEUPOGEN filgrastim and/or MOZOBIL® (plerixafor), after a minimum of 8 weeks of transfusions of packed red cells, to achieve a level of sickle hemoglobin of less than 30% in the patient with SCD. CTX001 was then manufactured from these CD34+ cells by editing with CRISPR-Cas9 with the use of a single-guide RNA molecule, following preclinical studies of BCL11A editing. Patients received myeloablation with pharmacokinetically adjusted, single-agent Busulfan, before the infusion of CTX001.
Eligible patients were between ages 18 and 35 years. In the CLIMB THAL-111 trial, eligible patients had a diagnosis of beta-Thalassemia (including the hemoglobin E genotype) with either homozygous or compound heterozygous mutations and had received transfusions of PRBC consisting of at least 100 ml/kg of body weight (or 10 units) per year during the previous 2 years. In the open-label CLIMB SCD-121 trial, eligible patients had a documented BS/BS or BS/B0 genotype and had a history of two or more severe vaso-occlusive episodes per year during the previous 2 years. Patients were monitored for engraftment, adverse events, total hemoglobin, hemoglobin fractions on high-performance liquid chromatography, F-cell expression (defined as the percentage of circulating erythrocytes with detectable levels of fetal hemoglobin), laboratory signs of hemolysis, requirements for transfusion support with PRBC, and occurrence of vaso-occlusive episodes in the patient with SCD. Bone marrow aspirates were obtained at 6 and 12 months after infusion, and DNA sequencing was used to measure the fraction of total DNA that was edited at the on-target site in CD34+ bone marrow cells and in nucleated peripheral-blood cells.
The Primary endpoint of the CLIMB THAL-111 trial was the proportion of patients with a transfusion reduction of 50% for at least six months, starting three months after CTX001 infusion. The Primary endpoint of CLIMB SCD-121 Sickle Cell Disease trial was the proportion of patients with fetal hemoglobin of 20% or more, sustained for at least three months, starting six months after CTX001 infusion.
CLIMB THAL-111 trial: Data was reported on 7 patients enrolled in the CLIMB THAL-111 trial, as they had reached at least three months of follow up after CTX001 infusion and therefore could be assessed for initial safety and efficacy. All seven showed a similar pattern of response, with rapid and sustained increases in total hemoglobin, fetal hemoglobin, and transfusion independence at last analysis. All 7 patients were transfusion independent with follow up ranging from 3-18 months after CTX001 infusion, with normal to near normal total hemoglobin levels at last visit. Their total hemoglobin levels ranged from 9.7 to 14.1 g/dL, and fetal hemoglobin ranged from 40.9% to 97.7%. Bone marrow allelic editing data collected from 4 patients with 6 months of follow up, and from one patient with 12 months of follow-up after CTX001 infusion showed the treatment resulted in a durable response. The safety data from all seven patients were generally consistent with an Autologous Stem Cell Transplant (ASCT) and myeloablative conditioning. There were four Serious Adverse Events (SAEs) considered related or possibly related to CTX001 reported in one patient and included headache, Hemophagocytic LymphoHistiocytosis (HLH), Acute Respiratory Distress Syndrome, and Idiopathic Pneumonia Syndrome. All four SAEs occurred in the context of HLH and resolved. Most of the non-SAEs were considered mild to moderate. CLIMB-111 is an ongoing trial and will enroll up to 45 patients and follow patients for approximately two years after infusion.
CLIMB SCD-121: Data was reported on 3 patients enrolled in the CLIMB SCD-121 sickle cell disease trial as they had reached at least three months of follow up after CTX001 infusion, and therefore could be assessed for initial safety and efficacy. Again, all 3 patients showed a similar pattern of response, with rapid and sustained increases in total hemoglobin and fetal hemoglobin, as well as elimination of Vaso-Occlusive Crises through last analysis. All 3 patients remained Vaso Occlusive Crises-free with follow up ranging from 3-15 months after CTX001 infusion and had hemoglobin levels in the normal to near normal range, including total hemoglobin from 11.5 to 13.2 g/dL and Fetal hemoglobin levels from 31.3% to 48.0%. Bone marrow allelic editing data collected from one patient with six months of follow-up and from one patient with 12 months of follow-up after CTX001 infusion demonstrated a durable response. Again the safety data were consistent with an ASCT and myeloablative conditioning. There were no Serious Adverse Events noted, thought to be related to CTX001, and the majority of non-SAEs were considered mild to moderate. CLIMB-121 is an ongoing open-label trial and will enroll up to 45 patients and follow patients for approximately two years after infusion.
It was concluded from this initial follow up that, CTX001 manufactured from Hematopoietic Stem Cells, edited of BCL11A with CRISPR-Cas9, has shown durable engraftment, with high levels of fetal hemoglobin expression, and the elimination of vaso-occlusive episodes or need for transfusion. The authors added that these preliminary results support further testing of CRISPR-Cas9 gene-editing approaches to treat other genetic diseases.
Safety and Efficacy of CTX001 in Patients with Transfusion-Dependent β- Thalassemia and Sickle Cell Disease: Early Results from the Climb THAL-111 and Climb SCD-121 Studies of Autologous CRISPR-CAS9–Modified CD34+ Hematopoietic Stem and Progenitor Cells. Frangoul H, Bobruff Y, Cappellini MD, et al. Presented at the 62nd ASH Annual Meeting and Exposition, 2020. Abstract#4