Cancer Pain (PDQ®)–Health Professional Version
General Information About Cancer Pain
Pain is one of the most common symptoms in cancer patients and often has a negative impact on patients’ functional status and quality of life (QOL). The goal of the following summary is to provide evidence-based, up-to-date, and practical information on the management of cancer pain.
Effective pain management can generally be accomplished by paying attention to the following steps:[1]
- Regular screening to ensure that the patient’s pain is recognized early. For more information, see the Pain Assessment section.
- Proper characterization of the pain to identify underlying pathophysiology, which could significantly influence treatment options. For more information, see the Pain Classification section.
- Is the pain acute or chronic?
- Is it secondary to cancer, cancer treatment, other causes, or a combination?
- Is it somatic, visceral, neuropathic, or mixed?
- Is there an incidental component?
- Is there breakthrough pain?
- Determining whether the pain requires pharmacological and/or other modalities of treatment. Pain is often multifactorial in nature, so factors that may modulate pain expression, such as psychological distress and substance use, should be assessed. For more information, see the Background and Definitions section.
- What is the impact of pain on the patient?
- Is the benefit of treatment likely going to outweigh the risks?
- Identifying the optimal pharmacological and nonpharmacological treatment options, including referrals to specialists, if needed. For more information, see the sections on Pharmacological Therapies for Pain Control and Modalities for Pain Control: Other Approaches. Complex pain often requires multidimensional interdisciplinary evaluation and intervention. There are many issues to consider when determining the most appropriate treatment, such as the following:
- Previous pain treatments.
- Patient prognosis.
- Predictive factors for pain control (e.g., psychological distress).
- Impact on function.
- Comorbidities (e.g., renal or hepatic failure).
- Risk of misuse of or addiction to pain medications.
- Patient preference.
- Providing proper education about treatment, including medication administration, expected side effects and associated treatments, and when patients can expect improvement. If opioids are considered, fear of opioids and the risks of opioid use and misuse should be addressed. Patients and family caregivers should be educated about the safe storage, use, and disposal of opioids. One study demonstrated that improper use, storage, and disposal are common among cancer outpatients.[2]
- Monitoring the patient longitudinally with return visits to titrate/adjust treatments. Patients with cancer or noncancer pain requiring chronic therapy are monitored closely to optimize treatment and to minimize the likelihood of complications of opioid use, including misuse or abuse. The risks and benefits of opioid use are evaluated regularly, and physician impressions are discussed openly with the patient.
Background and Definitions
The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”[3] Pain is commonly experienced by cancer patients. Its proper assessment requires the following:
- Measuring pain location(s), intensity, quality, and other factors.
- Clarifying the impact of pain on patients’ psychological, social, spiritual, and existential domains.
- Establishing treatment adherence and responsiveness.
Pain intensity may be assessed by asking patients to rate their pain on a numeric rating scale (NRS) of 0 to 10, with 0 defined as no pain and 10 defined as the worst pain imaginable. Although highly subjective, this scale may assist practitioners in gauging a patient’s pain status.[4] A commonly used approach to pain management employs the three-step World Health Organization pain relief ladder, which categorizes pain intensity according to severity and recommends analgesic agents based on their strength.[5]
Familiarity with opioid pharmacokinetics, equianalgesic dosing, and adverse effects is necessary for their safe and effective use. The appropriate use of adjuvant pharmacological and nonpharmacological interventions is needed to optimize pain management.
Prevalence
Pain occurs in 20% to 50% of patients with cancer.[6] Roughly 80% of patients with advanced-stage cancer have moderate to severe pain.[7] One meta-analysis looking at pooled data from 52 studies found that more than half of patients had pain.[8] Younger patients are more likely to experience cancer pain and pain flares than are older patients.[9]
Causes of Cancer Pain: Cancer, Cancer Treatments, and Comorbidities
A study evaluating the characteristics of patients (N = 100) with advanced cancer presenting to a palliative care service found the primary tumor as the chief cause of pain in 68% of patients.[10] Most pain was somatic, and pain was as likely to be continuous as intermittent.
Pain can be caused by the following:
- Surgery.
- Radiation therapy.
- Chemotherapy.
- Targeted therapy.
- Supportive care therapies.
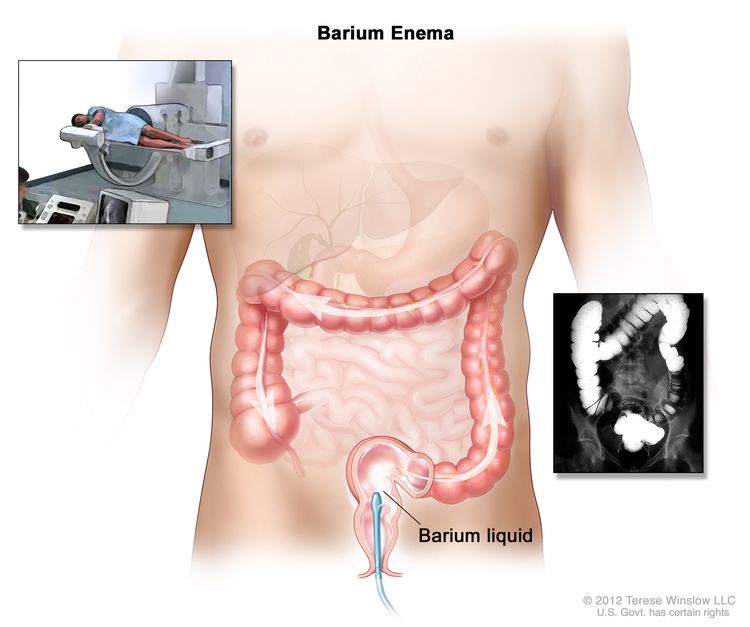
- Diagnostic procedures.
A systematic review of the literature identified reports of pain occurring in 59% of patients receiving anticancer treatment and in 33% of patients after curative treatments.[8] The prevalence of chronic nonmalignant pain—such as chronic low back pain, osteoarthritis pain, fibromyalgia, and chronic daily headaches—has not been well characterized in cancer patients. It has been reported to range from 2% to 76%, depending on the patient population and how pain was assessed.[11–14]
Postoperative pain
Pain is an expected consequence of surgery. Concerns about the prevalence of opioid misuse have drawn increasing attention to how opioids are prescribed in common settings, including postoperatively. Studies suggest widespread variation in the prescribing patterns of opioids in the postoperative setting.[15] One study of opioid use after orthopedic and general surgery procedures found that, on average, only between 19% and 34% of the opioids prescribed were used and that the quantity of opioids prescribed after a given procedure varied widely by provider.[15] This finding led to the evaluation of utilization data and recommendations for standardizing the quantity of opioids prescribed for five common general surgery procedures.[16] An educational intervention based on those recommendations was associated with a 53% decrease in prescribed opioids after those five general surgery procedures, with only 1 patient in a cohort of 246 patients requiring an opioid refill.[17]
The opioid epidemic has also raised questions about whether postoperative use of opioids can lead to misuse. New persistent opioid use develops in 6% to 8% of opioid-naïve patients after noncancer surgery.[18–20] In a large retrospective analysis of patients undergoing curative-intent cancer surgery, 10.4% of opioid-naïve patients developed new persistent opioid use, defined as filling opioid prescriptions 90 to 180 days after surgery. At 1 year postsurgery, these patients were using an average of six 5-mg hydrocodone (or equivalent) tablets per day. Among the risk factors evaluated, only the use of adjuvant chemotherapy increased the risk of new persistent opioid use (15%–21% risk with adjuvant chemotherapy vs. 7%–11% risk with no chemotherapy).[21] In summary, one in ten patients undergoing curative-intent cancer surgery may be at risk of postoperative persistent opioid use.
Infusion-related pain syndromes
The infusion of intravenous chemotherapy causes four pain syndromes:[22–24]
- Venous spasm, which is treated by the application of a warm compress or a decrease in the infusion rate.
- Chemical phlebitis, which may result from chemotherapy or nonchemotherapy infusions such as potassium chloride and hyperosmolar solutions.[23]
- Vesicant extravasation, which may cause intense pain followed by desquamation and ulceration.[22]
- Anthracycline-associated flare, a venous flare reaction that may be caused by doxorubicin and includes local urticaria, pain, or stinging.[24]
Some chemotherapy agents such as vinorelbine may cause pain at the tumor site.[25]
Treatment-related mucositis
Severe mucositis often occurs as a consequence of myeloablative chemotherapy and standard-intensity therapy.[26] Cytotoxic agents commonly associated with mucositis are cytarabine, doxorubicin, etoposide, fluorouracil (5-FU), and methotrexate. Epidermal growth factor receptor (EGFR) inhibitors, multitargeted tyrosine kinase inhibitors, and mammalian target of rapamycin inhibitors also cause mucositis.[27,28] Risk factors for mucositis include preexisting oral pathology, poor dental hygiene, and younger age.[26]
White blood cell growth factor–related bone pain
Filgrastim and pegfilgrastim are recombinant granulocyte colony-stimulating factors (G-CSFs) that increase proliferation and differentiation of neutrophil precursors. Ostealgia is a significant adverse effect caused by G-CSFs that can occur in 20% to 71% of patients.[29] This bone pain starts within 2 days of a pegfilgrastim dose and lasts for 2 to 4 days. Although the mechanism by which G-CSFs cause bone pain is largely unknown, it is hypothesized that histamine release, creating local inflammation and edema, may play a role. A phase II trial randomly assigned patients who had experienced bone pain with pegfilgrastim to receive either daily loratadine 10 mg for 7 days or matching placebo after subsequent doses of pegfilgrastim.[30] There was no statistically significant difference between the two arms.
A second phase II trial randomly assigned patients receiving pegfilgrastim to receive naproxen, loratadine, or no preventative medications.[31] The percentage of patients experiencing any grade bone pain was 40.3% in the naproxen group, 42.5% in the loratadine group, and 46.6% in the no-prophylaxis group. Although there was no statistically significant difference between treatment groups, the authors concluded that loratadine administration has a favorable risk-to-benefit profile and should be considered.
Conventional pain medications have also been studied in this area. A phase III, double-blind, placebo-controlled trial of naproxen for the prevention of pegfilgrastim-induced bone pain randomly assigned patients to receive either naproxen 500 mg twice daily for 5 to 8 days after pegfilgrastim administration or placebo.[32] Naproxen reduced overall pain intensity and duration of pain, compared with placebo.
Chemotherapy-related musculoskeletal pain
Paclitaxel generates a syndrome of diffuse arthralgias and myalgias in 10% to 20% of patients.[33] Diffuse pain in joints and muscles appears 1 to 2 days after the infusion and lasts a median of 4 to 5 days. Pain originates in the back, hips, shoulders, thighs, legs, and feet. Weight bearing, walking, or tactile contact exacerbates the pain. Steroids may reduce the tendency to develop myalgia and arthralgias. Among hormonal therapies, aromatase inhibitors cause musculoskeletal symptoms, osteoporotic fractures, arthralgias, and myalgias.[34]
Dermatologic complications and chemotherapy
EGFR inhibitors cause dermatitis with ensuing pain.[35] Acute herpetic neuralgia occurs with a significantly increased incidence among cancer patients, especially those with hematologic malignancies and those receiving immunosuppressive therapies.[36] The pain usually resolves within 2 months but can persist and become postherpetic neuralgia. The palmar-plantar erythrodysesthesia syndrome is observed in association with continuously infused 5-FU, capecitabine,[37] liposomal doxorubicin,[38] and paclitaxel.[39] Targeted agents such as sorafenib and sunitinib are also associated with hand-foot–like syndrome.[40] Patients develop tingling or burning in their palms and soles, followed by an erythematous rash. Management often requires discontinuing therapy or reducing the treatment dose.
Supportive care therapies and pain
Supportive care therapies can cause pain, as typified by bisphosphonate-associated osteonecrosis of the jaw.[41] Corticosteroid use has also been associated with the development of avascular necrosis.[42]
Radiation-induced pain
Radiation is associated with several distinct pain syndromes. First, patients may experience pain from brachytherapy and from positioning during treatment (i.e., placement on a radiation treatment table). Second, delayed tissue damage such as mucositis, mucosal inflammation in areas receiving radiation, and dermatitis may be painful. Third, a temporary worsening of pain in the treated area (a pain flare) is a potential side effect of radiation treatment for bone metastases.[43] A randomized trial demonstrated that dexamethasone (8 mg on day of radiation therapy and daily for the following 4 days) reduces the incidence of pain flares, compared with placebo.[44] For more information, see the External-Beam Radiation Therapy section.
Impact on Function and QOL
Cancer pain is associated with increased emotional distress. Both pain duration and pain severity correlate with risk of developing depression. Cancer patients are disabled an average of 12 to 20 days per month, with 28% to 55% unable to work because of their cancer.[45] Cancer survivors may experience distress when their pain unexpectedly persists after completion of cancer treatments.[46] Survivors also experience loss of support from their previous health care team as oncologists transition their care back to primary care providers.
In one study, between 20% and 50% of cancer patients continued to experience pain and functional limitations years posttreatment.[47] Untreated pain leads to requests for physician-assisted suicide.[48] Untreated pain also leads to unnecessary hospital admissions and visits to emergency departments.[49]
References
- Hui D, Bruera E: A personalized approach to assessing and managing pain in patients with cancer. J Clin Oncol 32 (16): 1640-6, 2014. [PUBMED Abstract]
- Reddy A, de la Cruz M, Rodriguez EM, et al.: Patterns of storage, use, and disposal of opioids among cancer outpatients. Oncologist 19 (7): 780-5, 2014. [PUBMED Abstract]
- Raja SN, Carr DB, Cohen M, et al.: The revised International Association for the Study of Pain definition of pain: concepts, challenges, and compromises. Pain 161 (9): 1976-1982, 2020. [PUBMED Abstract]
- Oldenmenger WH, de Raaf PJ, de Klerk C, et al.: Cut points on 0-10 numeric rating scales for symptoms included in the Edmonton Symptom Assessment Scale in cancer patients: a systematic review. J Pain Symptom Manage 45 (6): 1083-93, 2013. [PUBMED Abstract]
- Davis MP, Walsh D: Epidemiology of cancer pain and factors influencing poor pain control. Am J Hosp Palliat Care 21 (2): 137-42, 2004 Mar-Apr. [PUBMED Abstract]
- Fischer DJ, Villines D, Kim YO, et al.: Anxiety, depression, and pain: differences by primary cancer. Support Care Cancer 18 (7): 801-10, 2010. [PUBMED Abstract]
- Bruera E, Kim HN: Cancer pain. JAMA 290 (18): 2476-9, 2003. [PUBMED Abstract]
- van den Beuken-van Everdingen MH, de Rijke JM, Kessels AG, et al.: Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol 18 (9): 1437-49, 2007. [PUBMED Abstract]
- Green CR, Hart-Johnson T: Cancer pain: an age-based analysis. Pain Med 11 (10): 1525-36, 2010. [PUBMED Abstract]
- Gutgsell T, Walsh D, Zhukovsky DS, et al.: A prospective study of the pathophysiology and clinical characteristics of pain in a palliative medicine population. Am J Hosp Palliat Care 20 (2): 140-8, 2003 Mar-Apr. [PUBMED Abstract]
- Caraceni A, Portenoy RK: An international survey of cancer pain characteristics and syndromes. IASP Task Force on Cancer Pain. International Association for the Study of Pain. Pain 82 (3): 263-74, 1999. [PUBMED Abstract]
- Barbera L, Molloy S, Earle CC: Frequency of non-cancer-related pain in patients with cancer. J Clin Oncol 31 (22): 2837, 2013. [PUBMED Abstract]
- Childers JW, King LA, Arnold RM: Chronic Pain and Risk Factors for Opioid Misuse in a Palliative Care Clinic. Am J Hosp Palliat Care 32 (6): 654-9, 2015. [PUBMED Abstract]
- Massaccesi M, Deodato F, Caravatta L, et al.: Incidence and management of noncancer pain in cancer patients referred to a radiotherapy center. Clin J Pain 29 (11): 944-7, 2013. [PUBMED Abstract]
- Kim N, Matzon JL, Abboudi J, et al.: A Prospective Evaluation of Opioid Utilization After Upper-Extremity Surgical Procedures: Identifying Consumption Patterns and Determining Prescribing Guidelines. J Bone Joint Surg Am 98 (20): e89, 2016. [PUBMED Abstract]
- Hill MV, McMahon ML, Stucke RS, et al.: Wide Variation and Excessive Dosage of Opioid Prescriptions for Common General Surgical Procedures. Ann Surg 265 (4): 709-714, 2017. [PUBMED Abstract]
- Hill MV, Stucke RS, McMahon ML, et al.: An Educational Intervention Decreases Opioid Prescribing After General Surgical Operations. Ann Surg 267 (3): 468-472, 2018. [PUBMED Abstract]
- Clarke H, Soneji N, Ko DT, et al.: Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ 348: g1251, 2014. [PUBMED Abstract]
- Soneji N, Clarke HA, Ko DT, et al.: Risks of Developing Persistent Opioid Use After Major Surgery. JAMA Surg 151 (11): 1083-1084, 2016. [PUBMED Abstract]
- Brummett CM, Waljee JF, Goesling J, et al.: New Persistent Opioid Use After Minor and Major Surgical Procedures in US Adults. JAMA Surg 152 (6): e170504, 2017. [PUBMED Abstract]
- Lee JS, Hu HM, Edelman AL, et al.: New Persistent Opioid Use Among Patients With Cancer After Curative-Intent Surgery. J Clin Oncol 35 (36): 4042-4049, 2017. [PUBMED Abstract]
- Sauerland C, Engelking C, Wickham R, et al.: Vesicant extravasation part I: Mechanisms, pathogenesis, and nursing care to reduce risk. Oncol Nurs Forum 33 (6): 1134-41, 2006. [PUBMED Abstract]
- Pucino F, Danielson BD, Carlson JD, et al.: Patient tolerance to intravenous potassium chloride with and without lidocaine. Drug Intell Clin Pharm 22 (9): 676-9, 1988. [PUBMED Abstract]
- Curran CF, Luce JK, Page JA: Doxorubicin-associated flare reactions. Oncol Nurs Forum 17 (3): 387-9, 1990 May-Jun. [PUBMED Abstract]
- Long TD, Twillman RK, Cathers-Schiffman TA, et al.: Treatment of vinorelbine-associated tumor pain. Am J Clin Oncol 24 (4): 414-5, 2001. [PUBMED Abstract]
- Peterson DE, Lalla RV: Oral mucositis: the new paradigms. Curr Opin Oncol 22 (4): 318-22, 2010. [PUBMED Abstract]
- Lacouture ME, Anadkat MJ, Bensadoun RJ, et al.: Clinical practice guidelines for the prevention and treatment of EGFR inhibitor-associated dermatologic toxicities. Support Care Cancer 19 (8): 1079-95, 2011. [PUBMED Abstract]
- Boers-Doets CB, Epstein JB, Raber-Durlacher JE, et al.: Oral adverse events associated with tyrosine kinase and mammalian target of rapamycin inhibitors in renal cell carcinoma: a structured literature review. Oncologist 17 (1): 135-44, 2012. [PUBMED Abstract]
- Moore DC, Pellegrino AE: Pegfilgrastim-Induced Bone Pain: A Review on Incidence, Risk Factors, and Evidence-Based Management. Ann Pharmacother 51 (9): 797-803, 2017. [PUBMED Abstract]
- Moukharskaya J, Abrams DM, Ashikaga T, et al.: Randomized phase II study of loratadine for the prevention of bone pain caused by pegfilgrastim. Support Care Cancer 24 (7): 3085-93, 2016. [PUBMED Abstract]
- Kirshner JJ, McDonald MC, Kruter F, et al.: NOLAN: a randomized, phase 2 study to estimate the effect of prophylactic naproxen or loratadine vs no prophylactic treatment on bone pain in patients with early-stage breast cancer receiving chemotherapy and pegfilgrastim. Support Care Cancer 26 (4): 1323-1334, 2018. [PUBMED Abstract]
- Kirshner JJ, Heckler CE, Janelsins MC, et al.: Prevention of pegfilgrastim-induced bone pain: a phase III double-blind placebo-controlled randomized clinical trial of the university of rochester cancer center clinical community oncology program research base. J Clin Oncol 30 (16): 1974-9, 2012. [PUBMED Abstract]
- Loprinzi CL, Maddocks-Christianson K, Wolf SL, et al.: The Paclitaxel acute pain syndrome: sensitization of nociceptors as the putative mechanism. Cancer J 13 (6): 399-403, 2007 Nov-Dec. [PUBMED Abstract]
- Coleman RE, Bolten WW, Lansdown M, et al.: Aromatase inhibitor-induced arthralgia: clinical experience and treatment recommendations. Cancer Treat Rev 34 (3): 275-82, 2008. [PUBMED Abstract]
- Lynch TJ, Kim ES, Eaby B, et al.: Epidermal growth factor receptor inhibitor-associated cutaneous toxicities: an evolving paradigm in clinical management. Oncologist 12 (5): 610-21, 2007. [PUBMED Abstract]
- Portenoy RK, Duma C, Foley KM: Acute herpetic and postherpetic neuralgia: clinical review and current management. Ann Neurol 20 (6): 651-64, 1986. [PUBMED Abstract]
- Gressett SM, Stanford BL, Hardwicke F: Management of hand-foot syndrome induced by capecitabine. J Oncol Pharm Pract 12 (3): 131-41, 2006. [PUBMED Abstract]
- Alberts DS, Garcia DJ: Safety aspects of pegylated liposomal doxorubicin in patients with cancer. Drugs 54 (Suppl 4): 30-5, 1997. [PUBMED Abstract]
- Vukelja SJ, Baker WJ, Burris HA, et al.: Pyridoxine therapy for palmar-plantar erythrodysesthesia associated with taxotere. J Natl Cancer Inst 85 (17): 1432-3, 1993. [PUBMED Abstract]
- Chu D, Lacouture ME, Fillos T, et al.: Risk of hand-foot skin reaction with sorafenib: a systematic review and meta-analysis. Acta Oncol 47 (2): 176-86, 2008. [PUBMED Abstract]
- Prommer EE: Toxicity of bisphosphonates. J Palliat Med 12 (11): 1061-5, 2009. [PUBMED Abstract]
- Mattano LA, Devidas M, Nachman JB, et al.: Effect of alternate-week versus continuous dexamethasone scheduling on the risk of osteonecrosis in paediatric patients with acute lymphoblastic leukaemia: results from the CCG-1961 randomised cohort trial. Lancet Oncol 13 (9): 906-15, 2012. [PUBMED Abstract]
- Ripamonti CI, Bossi P, Santini D, et al.: Pain related to cancer treatments and diagnostic procedures: a no man’s land? Ann Oncol 25 (6): 1097-106, 2014. [PUBMED Abstract]
- Chow E, Meyer RM, Ding K, et al.: Dexamethasone in the prophylaxis of radiation-induced pain flare after palliative radiotherapy for bone metastases: a double-blind, randomised placebo-controlled, phase 3 trial. Lancet Oncol 16 (15): 1463-72, 2015. [PUBMED Abstract]
- Brown LF, Kroenke K, Theobald DE, et al.: The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Psychooncology 19 (7): 734-41, 2010. [PUBMED Abstract]
- Jim HS, Andersen BL: Meaning in life mediates the relationship between social and physical functioning and distress in cancer survivors. Br J Health Psychol 12 (Pt 3): 363-81, 2007. [PUBMED Abstract]
- Harrington CB, Hansen JA, Moskowitz M, et al.: It’s not over when it’s over: long-term symptoms in cancer survivors–a systematic review. Int J Psychiatry Med 40 (2): 163-81, 2010. [PUBMED Abstract]
- Foley KM: The relationship of pain and symptom management to patient requests for physician-assisted suicide. J Pain Symptom Manage 6 (5): 289-97, 1991. [PUBMED Abstract]
- Mayer DK, Travers D, Wyss A, et al.: Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 29 (19): 2683-8, 2011. [PUBMED Abstract]
Pain Classification
Total Pain
The concept of total pain captures its multidimensional nature by explicitly including the physical, psychological, social, and spiritual components of pain.[1–4] The immediate implications for the clinician are severalfold:
- A complete assessment of pain requires screening for psychological distress, social disruption, and existential crises, to treat the pain effectively and to anticipate barriers to pain relief.
- Patients’ descriptions of pain that seem out of proportion to the known pathology may reflect other syndromes such as depression and existential distress.[5]
- Patients suffering from pain often require multidimensional interventions from supportive services such as palliative care, chaplaincy, or psychotherapy.[6]
- The concept of total pain does not suggest that pain is solely caused by psychological or existential distress, but that psychological and spiritual components can exacerbate or ameliorate the experience of pain. If the clinician suspects somatization, then referral for psychiatric or psychological evaluation is indicated.
Pain Mechanisms
Pain is classified on the basis of the underlying pathophysiologic mechanisms, the duration, or the description of recognizable syndromes associated with pain.[7] The three mechanisms underlying the pathophysiology of pain are:
- Nociceptive.
- Neuropathic.
Nociceptive pain, which may be either somatic or visceral in nature, originates with a chemical, mechanical, or thermal injury to tissue that stimulates pain receptors that transmit a signal to the central nervous system (CNS), causing the perception of pain. Pain receptors are found in somatic (e.g., cutaneous, bone) and visceral tissues. The amount of visceral sensory innervation and the diffusion of visceral pain signals within the brain explain the difficulty experienced by patients in describing or localizing visceral pain compared with somatic pain. A specific type of visceral pain is referred pain, which is explained by the commingling of nerve fibers from somatic and visceral nociceptors at the level of the spinal cord. Patients mistakenly interpret the pain as originating from the innervated somatic tissue. Visceral pain may be accompanied by autonomic signs such as sweating, pallor, or bradycardia. Somatic pain is more easily localized.
Neuropathic pain is pain caused by damage to the peripheral nervous system or the CNS (spinal cord or brain). Causes of neuropathic pain of particular relevance to cancer include chemotherapy (e.g., vinca alkaloids), infiltration of the nerve roots by tumor, or damage to nerve roots (radiculopathy) or groups of nerve roots (plexopathy) due to tumor masses or treatment complications (e.g., radiation plexopathy).[8] The pain may be evoked by stimuli or spontaneous. Patients who experience pain from nonnoxious stimuli are classified as having allodynia. Hyperalgesia connotes increased sensations of pain out of proportion to what is usually experienced.
Emotional distress may also contribute to the pain experience. Most patients with cancer and pain do not have somatic symptom disorder. However, if pain complaints appear to be disproportionate to the underlying pain stimulus, it is important to evaluate for psychological and existential distress contributing to the pain complaint, chemical coping, and substance use disorder.
Acute and Chronic Cancer Pain
Pain is often classified as either acute or chronic or by how it varies over time with terms such as breakthrough, persistent, or incidental. Acute pain is typically induced by tissue injury, begins suddenly with the injury, and diminishes over time with tissue healing. There is no definite length but, in general, acute pain resolves within 3 to 6 months.[9] The treatment of acute pain focuses on blocking nociceptive pathways while the tissue heals.
Chronic pain typically persists even after the injury has healed, although patients with chronic joint disease, for example, may have ongoing tissue damage and therefore experience chronic pain. Pain becomes chronic when it:[9]
- Continues for more than 1 month after the healing of precipitating lesions.
- Persists or becomes recurrent over months.
- Results from lesions unlikely to regress or heal.
The transition from acute to chronic pain may be understood as a series of relatively discrete changes in the CNS,[9] but the genesis of chronic pain also includes clearly behavioral confounders. Chronic pain involves the activation of secondary mechanisms such as the sensitization of second-order neurons by upregulation of N-methyl-D-aspartic acid channels and alteration in microglia cytoarchitecture. Chronic pain, with its multiple factors for perpetuation, often benefits from a multidisciplinary approach to treatment.
Breakthrough Pain
In caring for patients with pain, breakthrough pain is distinguished from background pain.[10,11] Breakthrough pain is a transitory increase or flare of pain in the setting of relatively well-controlled acute or chronic pain.[12] Incident pain is a type of breakthrough pain related to certain often-defined activities or factors such as movement increasing vertebral body pain from metastatic disease. It is often difficult to treat such pain effectively because of its episodic nature.[13] In one study, 75% of patients experienced breakthrough pain; 30% of this pain was incidental, 26% was nonincidental, 16% was caused by end-of-dose failure, and the rest had mixed etiologies.[14]
References
- Richmond C: Dame Cicely Saunders. Br Med J 331 (7510): 238, 2005. Also available online. Last accessed Feb. 9, 2024.
- Mehta A, Chan LS: Understanding of the concept of “total pain”: a prerequisite for pain control. J Hosp Palliat Nurs 10 (1): 26-32, 2008.
- Syrjala KL, Jensen MP, Mendoza ME, et al.: Psychological and behavioral approaches to cancer pain management. J Clin Oncol 32 (16): 1703-11, 2014. [PUBMED Abstract]
- Merskey H, Bogduk N, eds.: Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms. 2nd ed. IASP Press, 1994. Also available online. Last accessed Feb. 9, 2024.
- Porter LS, Keefe FJ: Psychosocial issues in cancer pain. Curr Pain Headache Rep 15 (4): 263-70, 2011. [PUBMED Abstract]
- Wachholtz A, Makowski S: Spiritual dimensions of pain and suffering. In: Moore RJ, ed.: Handbook of Pain and Palliative Care: Biobehavioral Approaches for the Life Course. Springer, 2013, pp 697-713.
- Chang VT, Janjan N, Jain S, et al.: Update in cancer pain syndromes. J Palliat Med 9 (6): 1414-34, 2006. [PUBMED Abstract]
- Dworkin RH, Backonja M, Rowbotham MC, et al.: Advances in neuropathic pain: diagnosis, mechanisms, and treatment recommendations. Arch Neurol 60 (11): 1524-34, 2003. [PUBMED Abstract]
- Voscopoulos C, Lema M: When does acute pain become chronic? Br J Anaesth 105 (Suppl 1): i69-85, 2010. [PUBMED Abstract]
- Portenoy RK, Hagen NA: Breakthrough pain: definition, prevalence and characteristics. Pain 41 (3): 273-81, 1990. [PUBMED Abstract]
- Narayana A, Katz N, Shillington AC, et al.: National Breakthrough Pain Study: prevalence, characteristics, and associations with health outcomes. Pain 156 (2): 252-9, 2015. [PUBMED Abstract]
- Caraceni A, Martini C, Zecca E, et al.: Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliat Med 18 (3): 177-83, 2004. [PUBMED Abstract]
- Mercadante S: Managing difficult pain conditions in the cancer patient. Curr Pain Headache Rep 18 (2): 395, 2014. [PUBMED Abstract]
- Gutgsell T, Walsh D, Zhukovsky DS, et al.: A prospective study of the pathophysiology and clinical characteristics of pain in a palliative medicine population. Am J Hosp Palliat Care 20 (2): 140-8, 2003 Mar-Apr. [PUBMED Abstract]
Pain Assessment
Patient-Reported Outcomes
Effective pain treatment begins with screening at every visit and a thorough assessment if pain is present. Patient self-report is the standard of care for evaluating pain.[1]
Many tools have been developed to quantify the intensity of pain. The most commonly used tools include the following:
- Numerical rating scale (0–10: 0 = no pain, 10 = worst pain imaginable).
- Categorical scale (none, mild, moderate, severe).
- Visual analog scale (0–100 mm: 0 mm = no pain, 100 mm = worst pain imaginable).
Multidimensional pain assessment tools such as the McGill Pain Questionnaire, the Brief Pain Inventory,[2] and the PROMIS-PI (Patient-Reported Outcomes Measurement Information System—Pain Interference) [3] have been developed to evaluate pain and its interference with daily functions. Although these tools are important, they may be best applied in the research setting, given their complexity and significant time requirements.
Pain assessment tools have been developed for special populations such as children and those with cognitive impairment. For more information, see the Special Considerations section.
Pain intensity may be assessed for different time frames, such as “now,” “last 24 hours,” or “last week.” In addition to the average pain intensity, the worst or lowest intensity may be assessed. Evaluation of pain intensity at each visit would allow clinicians to monitor for changes and treatment response. Pain intensity scales can also be used to develop a personalized pain goal (PPG).[4] A PPG is a patient’s self-reported pain management goal on a scale of 0 to 10 and is used to identify the maximum pain intensity that the patient considers tolerable.[5] The PPG is a relatively simple tool with a sensitivity of 83% and specificity of 77% when used for measuring pain relief.[6]
Patient-reported symptoms and clinician-assessed pain reporting may not be concordant, and discrepancies in assessment or interpretation of symptoms can be important in making decisions about cancer treatment. In one study, breast cancer patients who were undergoing an exercise intervention and who received four different chemotherapy regimens (e.g., anthracycline- and paclitaxel-based regimens) were assessed for symptoms of chemotherapy-induced peripheral neuropathy (CIPN) by patient self-report (the Patient-Reported Symptom Monitoring form, a five-point symptom scale) and by clinician assessment (the Common Terminology Criteria for Adverse Events form, a five-point adverse event rating scale).[7] Patient-reported pain symptoms were compared for concordance with clinician-assessed adverse events, and there was minimal agreement (weighted Cohen kappa, 0.34) between patient-reported and clinician-assessed CIPN toxicity scores. The discrepancy between patient-reported and clinician-assessed CIPN underscores the need for both patient and clinician perspectives regarding this common and potentially disabling toxicity of chemotherapy for patients with breast cancer. Treatment changes and reduced doses of anthracycline- and paclitaxel-based regimens could be driven by the inclusion of patient-reported symptoms, which may serve as a better indicator of CIPN toxicities.
Clinician Assessment
Failure to assess pain adequately leads to undertreatment. Assessment involves both clinician observation and patient report. The goal of the initial pain assessment is to characterize the pathophysiology of the pain and to determine the intensity of the pain and its impact on the patient’s ability to function. It is important to recognize that psychosocial issues can either exacerbate or ameliorate the experience of pain.[8] These psychosocial issues cannot be easily treated through pharmacological approaches; therefore, it is critical that clinicians include these in initial and subsequent examinations of patients with pain to ensure referrals to appropriate treatment resources. Furthermore, distinct cultural components may need to be incorporated into a multidimensional assessment of pain, including how culture influences the pain experience, pain communication, and provider response to pain expression.[9–12]
Identifying the etiology of pain is important for its management. Clinicians treating patients with cancer need to recognize the common cancer pain syndromes. For more information, see the sections on Approach to Somatic Pain, Approach to Visceral Pain, and Approach to Neuropathic Pain.
Effective pain management requires close monitoring of patient response after treatment is initiated. In a review of 1,612 patients referred to an outpatient palliative care center, more than half of patients with moderate to severe pain did not show pain relief (a reduction in 2 out of 10 points or a 30% decrease on the pain scale) after the initial palliative care consultation.[13] In addition, one-third of patients with mild pain progressed to moderate to severe pain by the time of their first follow-up visit. The study also identified baseline pain intensity, fatigue, and Edmonton Symptom Assessment System symptom burden as factors predicting response.[13]
Ideally, comprehensive pain assessment includes a discussion about the patient’s goals and expectations for pain management. This conversation may lead to a fruitful discussion about balancing pain levels and other patient goals, such as mental alertness. Comprehensive pain assessment also includes pain history, pain intensity, quality of pain, and location of pain. For each pain location, the pattern of pain radiation is assessed. Also important is provider awareness of the patient’s current pain management treatment plan and how the patient has responded to treatment; this includes how adequately the current treatment plan addresses any breakthrough or episodic pain. A full assessment also reviews previously attempted pain therapies and reasons for discontinuation; other associated symptoms such as sleep difficulties, fatigue, depression, and anxiety; functional impairment; and any relevant laboratory data and diagnostic imaging. A focused physical examination includes clinical observation of pain behaviors, pain location, and functional limitations.
Psychosocial and existential factors that can affect pain are also assessed and appropriately treated. Depression and anxiety can have a large influence on the pain experience. Across many different types of pain, research has shown the importance of considering a patient’s sense of self-efficacy over their pain: low self-efficacy, or focus on solely pharmacological solutions, is likely to increase the use of pain medication.[14,15] In addition, the psychological strategy of catastrophizing, an irrational thinking pattern that the outcome of any experience will always be significantly worse than what is the most likely outcome, has consistently been shown to escalate pain. Patients who repeatedly catastrophize pain (e.g., patient reports pain higher than 10 on a 10-point scale [“My pain is a 12!”] or believes that every minor, nonspecific symptom indicates a cancer recurrence [16]) are more likely to require higher doses of medication than are patients who do not catastrophize. Catastrophizing is strongly associated with low self-efficacy and greater reliance on chemical coping strategies.[16–20] Furthermore, assessing the impact of pain on the individual’s life and associated factors that exacerbate or relieve pain can reveal how psychosocial issues are affecting the patient’s pain levels.
A pain assessment includes a review of any patient and family history of substance use and the extent of the patient’s chemical coping strategies before and since the cancer diagnosis. The extent of chemical coping strategies, including reliance on legal substances (e.g., nicotine, alcohol, and sleeping pills), may indicate a history of reliance on chemicals to alleviate distress. It can also provide the clinician with information about the patient’s nicotine use, which may affect how certain opioids may be differentially metabolized and the amount of opioids required to achieve pain control.[21] A remote history of substance use disorder can still affect current pain levels and analgesic requirements. Remote substance use may have long-term implications for pain sensitivity, even if the patient has a history of prolonged abstinence from opioid use.[22] Together, personal and family substance use can inform a risk assessment for potential abuse of medications, potential analgesic requirements, and diversion of prescriptions.
Pain Prognostic Scores
Several pain-related factors and patient-related factors predict response to pain treatment. Specifically, a high baseline pain intensity, neuropathic pain, and incident pain are often more difficult to manage.[23] Furthermore, several patient characteristics are associated with higher pain expression, higher opioid doses, and longer time to achieve pain control. These characteristics include a personal or family history of the following:
On the basis of these predictive factors, several risk scores have been developed to assist clinicians in clinical practice, such as the Edmonton Classification System for Cancer Pain (ECS-CP) [23,34] and the Cancer Pain Prognostic Scale (CPPS).[35]
- The ECS-CP consists of (1) neuropathic pain, (2) incident pain, (3) psychological distress, (4) addiction, and (5) cognitive impairment. The presence of any of these factors indicates that pain may be more difficult to control. The ECS-CP has been validated in various cancer pain settings.[36]
- The CPPS includes four variables in a formula to determine the risk score, including worst pain severity (Brief Pain Inventory), Functional Assessment of Cancer Therapy – General (FACT-G) emotional well-being, initial morphine equivalent daily dose (≤60 mg/day; >60 mg/day), and mixed pain syndrome. The CPPS score ranges from 0 to 17, with a higher score indicating a higher possibility of pain relief.
Predictive factors can help to personalize cancer pain management. Especially for patients with a poor pain prognosis, clinicians may consider discussing realistic goals for alleviating pain, focusing on function and use of multimodality interventions. Repeated or frequent escalation of analgesic doses without improvement of pain may trigger clinicians to consider an alternative approach to pain.
Special Considerations
Self-report is accepted as the gold standard of pain assessment. However, for certain vulnerable populations, such as children, those with learning disabilities, and those who are cognitively impaired, self-report may not be feasible or reliable. An awareness of cultural perceptions and reporting of pain is also useful.
Children
While adults and children older than 7 years can effectively use the numerical rating scale, younger children and those with cognitive impairment may benefit from using a pictorial scale such as the Faces Pain Scale.[37]
Cognitive impairment
Cognitive impairment may impede a person’s ability to describe pain, recall pain events, or understand the tools used to assess pain. This can lead these patients to receive more or less analgesia than appropriate.[38–40] The American Society for Pain Management Nursing’s position statement on pain assessment in the nonverbal patient includes clinical recommendations.[41] Pain assessment can be evaluated via direct observation, family/caregiver report, and evaluation of response to pain relief interventions. For patients with advanced dementia, there are tools that rely on professional caregiver assessment of pain through the observation of patient behaviors.[42–44] Although the validity and reliability of these tools have been questioned, they are often recommended for patients with advanced dementia who cannot report pain. In combination with self-report by other cognitively impaired groups, these tools can enhance pain assessment and avoid undertreatment of pain.
Cognitive impairment extends beyond patients with dementia to those with brain tumors and delirium, which are common complications of advanced cancer. In such patients, the Faces Pain Scale [45] and the Coloured Analogue Scale, [46] as well as vertical instead of horizontal orientation of scales, may be preferable to the numerical rating scales.[47]
Culture
Culture also plays a role in patients’ experience and reporting of pain. For example, in some Asian cultures, patients tend not to report pain.[9] Complaining of pain may be perceived as a sign of weakness. Individuals may hide pain from family members to avoid burdening them. For some patients, pain may have spiritual value, leading them to accept pain rather than dull the experience with medication.[48] Thus, understanding an individual patient’s spiritual and cultural background, without making assumptions, is important in approaching pain assessment.
In a cross-sectional study, the cancer pain experience of White patients was individual and independent, while that of racial and ethnic minority patients was family oriented. Minority patients received support from their families during cancer treatment, and they fought cancer for their families. The families were involved deeply in decisions related to cancer treatment and pain management.[10] Other studies indicate that Asian patients have greater barriers to pain management and display more fatalism than Western patients.[11,12]
These studies describe larger cultural responses to pain that may inform assessments or improve understanding of pain communication by providers. It should be noted that subcultural differences or individual differences within each racial and ethnic group may affect the experience or expression of pain.
References
- Jensen MP, Karoly P: Measurement of cancer pain via patient self-report. In: Chapman CR, Foley KM, eds.: Current and Emerging Issues in Cancer Pain: Research and Practice. Raven Press, 1993, pp 193-218.
- Hølen JC, Lydersen S, Klepstad P, et al.: The Brief Pain Inventory: pain’s interference with functions is different in cancer pain compared with noncancer chronic pain. Clin J Pain 24 (3): 219-25, 2008 Mar-Apr. [PUBMED Abstract]
- Amtmann D, Cook KF, Jensen MP, et al.: Development of a PROMIS item bank to measure pain interference. Pain 150 (1): 173-82, 2010. [PUBMED Abstract]
- Dalal S, Hui D, Nguyen L, et al.: Achievement of personalized pain goal in cancer patients referred to a supportive care clinic at a comprehensive cancer center. Cancer 118 (15): 3869-77, 2012. [PUBMED Abstract]
- Tagami K, Okizaki A, Miura T, et al.: Breakthrough Cancer Pain Influences General Activities and Pain Management: A Comparison of Patients with and without Breakthrough Cancer Pain. J Palliat Med 21 (11): 1636-1640, 2018. [PUBMED Abstract]
- Arthur J, Tanco K, Park M, et al.: Personalized Pain Goal as an Outcome Measure in Routine Cancer Pain Assessment. J Pain Symptom Manage 56 (1): 80-87, 2018. [PUBMED Abstract]
- Nyrop KA, Deal AM, Reeder-Hayes KE, et al.: Patient-reported and clinician-reported chemotherapy-induced peripheral neuropathy in patients with early breast cancer: Current clinical practice. Cancer 125 (17): 2945-2954, 2019. [PUBMED Abstract]
- Turk DC, Okifuji A: Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol 70 (3): 678-90, 2002. [PUBMED Abstract]
- Duke G, Petersen S: Perspectives of Asians living in Texas on pain management in the last days of life. Int J Palliat Nurs 21 (1): 24-34, 2015. [PUBMED Abstract]
- Im EO, Lee SH, Liu Y, et al.: A national online forum on ethnic differences in cancer pain experience. Nurs Res 58 (2): 86-94, 2009 Mar-Apr. [PUBMED Abstract]
- Chen CH, Tang ST, Chen CH: Meta-analysis of cultural differences in Western and Asian patient-perceived barriers to managing cancer pain. Palliat Med 26 (3): 206-21, 2012. [PUBMED Abstract]
- Edrington J, Sun A, Wong C, et al.: Barriers to pain management in a community sample of Chinese American patients with cancer. J Pain Symptom Manage 37 (4): 665-75, 2009. [PUBMED Abstract]
- Yennurajalingam S, Kang JH, Hui D, et al.: Clinical response to an outpatient palliative care consultation in patients with advanced cancer and cancer pain. J Pain Symptom Manage 44 (3): 340-50, 2012. [PUBMED Abstract]
- Rokke PD, Fleming-Ficek S, Siemens NM, et al.: Self-efficacy and choice of coping strategies for tolerating acute pain. J Behav Med 27 (4): 343-60, 2004. [PUBMED Abstract]
- Keefe FJ, Abernethy AP, C Campbell L: Psychological approaches to understanding and treating disease-related pain. Annu Rev Psychol 56: 601-30, 2005. [PUBMED Abstract]
- Bishop SR, Warr D: Coping, catastrophizing and chronic pain in breast cancer. J Behav Med 26 (3): 265-81, 2003. [PUBMED Abstract]
- Wilson JM, Schreiber KL, Mackey S, et al.: Increased pain catastrophizing longitudinally predicts worsened pain severity and interference in patients with chronic pain and cancer: A collaborative health outcomes information registry study (CHOIR). Psychooncology 31 (10): 1753-1761, 2022. [PUBMED Abstract]
- Lukkahatai N, Saligan LN: Association of catastrophizing and fatigue: a systematic review. J Psychosom Res 74 (2): 100-9, 2013. [PUBMED Abstract]
- Syrjala KL, Jensen MP, Mendoza ME, et al.: Psychological and behavioral approaches to cancer pain management. J Clin Oncol 32 (16): 1703-11, 2014. [PUBMED Abstract]
- Schreiber KL, Martel MO, Shnol H, et al.: Persistent pain in postmastectomy patients: comparison of psychophysical, medical, surgical, and psychosocial characteristics between patients with and without pain. Pain 154 (5): 660-8, 2013. [PUBMED Abstract]
- Skurtveit S, Furu K, Selmer R, et al.: Nicotine dependence predicts repeated use of prescribed opioids. Prospective population-based cohort study. Ann Epidemiol 20 (12): 890-7, 2010. [PUBMED Abstract]
- Wachholtz A, Gonzalez G: Co-morbid pain and opioid addiction: long term effect of opioid maintenance on acute pain. Drug Alcohol Depend 145: 143-9, 2014. [PUBMED Abstract]
- Fainsinger RL, Fairchild A, Nekolaichuk C, et al.: Is pain intensity a predictor of the complexity of cancer pain management? J Clin Oncol 27 (4): 585-90, 2009. [PUBMED Abstract]
- Kwon JH, Hui D, Chisholm G, et al.: Predictors of long-term opioid treatment among patients who receive chemoradiation for head and neck cancer. Oncologist 18 (6): 768-74, 2013. [PUBMED Abstract]
- Parsons HA, Delgado-Guay MO, El Osta B, et al.: Alcoholism screening in patients with advanced cancer: impact on symptom burden and opioid use. J Palliat Med 11 (7): 964-8, 2008. [PUBMED Abstract]
- Dev R, Parsons HA, Palla S, et al.: Undocumented alcoholism and its correlation with tobacco and illegal drug use in advanced cancer patients. Cancer 117 (19): 4551-6, 2011. [PUBMED Abstract]
- Hooten WM, Townsend CO, Bruce BK, et al.: The effects of smoking status on opioid tapering among patients with chronic pain. Anesth Analg 108 (1): 308-15, 2009. [PUBMED Abstract]
- John U, Alte D, Hanke M, et al.: Tobacco smoking in relation to analgesic drug use in a national adult population sample. Drug Alcohol Depend 85 (1): 49-55, 2006. [PUBMED Abstract]
- Bener A, Verjee M, Dafeeah EE, et al.: Psychological factors: anxiety, depression, and somatization symptoms in low back pain patients. J Pain Res 6: 95-101, 2013. [PUBMED Abstract]
- Galloway SK, Baker M, Giglio P, et al.: Depression and Anxiety Symptoms Relate to Distinct Components of Pain Experience among Patients with Breast Cancer. Pain Res Treat 2012: 851276, 2012. [PUBMED Abstract]
- Bruera E, MacMillan K, Hanson J, et al.: The Edmonton staging system for cancer pain: preliminary report. Pain 37 (2): 203-9, 1989. [PUBMED Abstract]
- Bruera E, Schoeller T, Wenk R, et al.: A prospective multicenter assessment of the Edmonton staging system for cancer pain. J Pain Symptom Manage 10 (5): 348-55, 1995. [PUBMED Abstract]
- Delgado-Guay MO, Yennurajalingam S, Bruera E: Delirium with severe symptom expression related to hypercalcemia in a patient with advanced cancer: an interdisciplinary approach to treatment. J Pain Symptom Manage 36 (4): 442-9, 2008. [PUBMED Abstract]
- Fainsinger RL, Nekolaichuk CL, Lawlor PG, et al.: A multicenter study of the revised Edmonton Staging System for classifying cancer pain in advanced cancer patients. J Pain Symptom Manage 29 (3): 224-37, 2005. [PUBMED Abstract]
- Hwang SS, Chang VT, Fairclough DL, et al.: Development of a cancer pain prognostic scale. J Pain Symptom Manage 24 (4): 366-78, 2002. [PUBMED Abstract]
- Fainsinger RL, Nekolaichuk CL: A “TNM” classification system for cancer pain: the Edmonton Classification System for Cancer Pain (ECS-CP). Support Care Cancer 16 (6): 547-55, 2008. [PUBMED Abstract]
- Hicks CL, von Baeyer CL, Spafford PA, et al.: The Faces Pain Scale-Revised: toward a common metric in pediatric pain measurement. Pain 93 (2): 173-83, 2001. [PUBMED Abstract]
- Chatterjee J: Improving pain assessment for patients with cognitive impairment: development of a pain assessment toolkit. Int J Palliat Nurs 18 (12): 581-90, 2012. [PUBMED Abstract]
- Morrison RS, Siu AL: A comparison of pain and its treatment in advanced dementia and cognitively intact patients with hip fracture. J Pain Symptom Manage 19 (4): 240-8, 2000. [PUBMED Abstract]
- Buffum MD, Hutt E, Chang VT, et al.: Cognitive impairment and pain management: review of issues and challenges. J Rehabil Res Dev 44 (2): 315-30, 2007. [PUBMED Abstract]
- Herr K, Coyne PJ, Ely E, et al.: ASPMN 2019 Position Statement: Pain Assessment in the Patient Unable to Self-Report. Pain Manag Nurs 20 (5): 402-403, 2019. [PUBMED Abstract]
- Warden V, Hurley AC, Volicer L: Development and psychometric evaluation of the Pain Assessment in Advanced Dementia (PAINAD) scale. J Am Med Dir Assoc 4 (1): 9-15, 2003 Jan-Feb. [PUBMED Abstract]
- Fuchs-Lacelle S, Hadjistavropoulos T: Development and preliminary validation of the pain assessment checklist for seniors with limited ability to communicate (PACSLAC). Pain Manag Nurs 5 (1): 37-49, 2004. [PUBMED Abstract]
- Regnard C, Reynolds J, Watson B, et al.: Understanding distress in people with severe communication difficulties: developing and assessing the Disability Distress Assessment Tool (DisDAT). J Intellect Disabil Res 51 (Pt 4): 277-92, 2007. [PUBMED Abstract]
- Bieri D, Reeve RA, Champion GD, et al.: The Faces Pain Scale for the self-assessment of the severity of pain experienced by children: development, initial validation, and preliminary investigation for ratio scale properties. Pain 41 (2): 139-50, 1990. [PUBMED Abstract]
- McGrath PA, Seifert CE, Speechley KN, et al.: A new analogue scale for assessing children’s pain: an initial validation study. Pain 64 (3): 435-43, 1996. [PUBMED Abstract]
- Kremer E, Atkinson JH, Ignelzi RJ: Measurement of pain: patient preference does not confound pain measurement. Pain 10 (2): 241-8, 1981. [PUBMED Abstract]
- Ferrell B: Ethical perspectives on pain and suffering. Pain Manag Nurs 6 (3): 83-90, 2005. [PUBMED Abstract]
Pharmacological Therapies for Pain Control
Acetaminophen and Nonsteroidal Anti-inflammatory Drugs (NSAIDs)
Often initiated when an individual has mild pain, acetaminophen and NSAIDs are useful in managing moderate and severe pain as adjunct agents to opioids (see Table 1 and Table 3). No single NSAID is preferred over others, and all are better than placebo for analgesia.[1] As opioid adjuncts, acetaminophen and NSAIDs have shown benefit both in improved analgesia and in decreased opioid use. These agents are used with care or perhaps avoided in older patients or those who have renal, hepatic, or cardiac disease.[1] For more information, see the Geriatric cancer patients section in Treatment of Pain in Specific Patient Populations.
While acetaminophen and NSAIDs provide analgesia on their own, a number of randomized controlled trials have reported that the addition of either agent to opioids may improve pain control and decrease opioid need in cancer patients.[2–4] However, these benefits were not consistently observed across trials.[5,6]
High-potency NSAIDs such as ketorolac and diclofenac are more studied and have shown benefit in the management of cancer pain. However, there are no comparative data with older agents to show superiority of one product over others. Prominent side effects are gastrointestinal irritation, ulcer formation, and dyspepsia. Other side effects of concern include cardiotoxicity, nephrotoxicity, hepatotoxicity, and hematologic effects.[7,8] Cyclooxygenase-2 (COX-2)–specific agents such as celecoxib may have a more favorable gastrointestinal side effect profile at a higher monetary cost.[7] Long-term safety and efficacy data remain unclear.
| Drug | Dosage | Comments | Reference(s) |
|---|---|---|---|
| COX-2 = cyclooxygenase-2; GI = gastrointestinal; IM = intramuscular; IV = intravenous; NSAIDs = nonsteroidal anti-inflammatory drugs; PO = by mouth. | |||
| Acetaminophen | <4,000 mg/d | Dosed every 4 to 8 hours, depending on dose and product used. | [2] |
| Celecoxib | 200–400 mg/d | COX-2 specific. Minimal antiplatelet effects compared with nonselective NSAIDs. | [7] |
| Diclofenac | 100–200 mg/d | Available as immediate- and delayed/extended–release products. | [9] |
| Ibuprofen | 600–2,400 mg/d | [9] | |
| Ketoprofen | 100–300 mg/d | Available as parenteral in some parts of the world, which may be preferred. | [7,10] |
| Ketorolac | 40–60 mg/d, generally dosed every 6 hours | Parenteral (IV, IM) ketorolac is used ≤5 days because of concerns about GI adverse events. May also be given PO. | [7] |
Opioids
General principles
The use of opioids for the relief of moderate to severe cancer pain is considered necessary for most patients.[1] For more information, see Table 2 and Table 3.
- For moderate pain, weak opioids (e.g., codeine or tramadol) or lower doses of strong opioids (e.g., morphine, oxycodone, or hydromorphone) are often administered and frequently combined with nonopioid analgesics.[1]
- For severe pain, strong opioids are routinely used. Although no agent appears to be more effective than another, morphine is often considered the opioid of choice because of provider familiarity, broad availability, and lower cost.[1]
In one well-designed review, most individuals with moderate to severe cancer pain obtained significant pain relief from oral morphine.[11] One study has also noted that low-dose morphine (up to 30 mg orally per day) provided better analgesia than did weak opioids (codeine, tramadol).[12] A 2022 update to a Cochrane review of oxycodone for cancer-related pain concluded that there were no differences in pain intensity, pain relief, and adverse effects between oxycodone and other strong opioids, including morphine. However, based on low certainty of evidence, constipation and hallucinations occurred less often with long-acting oxycodone than with long-acting morphine.[13]
The management of acute pain begins with an immediate-release opioid formulation. Once pain is stabilized, opioid consumption is converted to a modified-release or longer-acting opioid on the basis of the patient’s previous 24-hour opioid consumption. The morphine milligram equivalent (MME) can then be used to convert to an alternative opioid, if desired. Randomized controlled trials have shown that long-acting opioids given every 12 hours provide efficacy similar to that of scheduled short-acting opioids given every 4 hours.[14,15] The dosing of long-acting opioids may lead to increased adherence. This finding is based on evidence from a cross-sectional study showing that analgesic medications taken at longer dose intervals (e.g., 8, 12, or 24 hours) were associated with increased adherence (P < .001), adjusting for pain, symptom, demographic, and setting variables in the model.[16] Use of the immediate-release product is continued for the management of breakthrough pain.[1]
During ongoing pain management, the immediate-release opioids inform the titration of long-acting medications. Rapid-acting oral, buccal, sublingual, transmucosal, rectal, and intranasal products are all acceptable for the treatment of breakthrough pain. In people who are unable to take oral medications, a subcutaneous method of delivery is as effective as the intravenous route for morphine and hydromorphone.
| Opioid Drug | Equianalgesic Dosing | Comments | Reference(s) |
|---|---|---|---|
| Buprenorphine | No consensus. | Transdermal product and sublingual available. May cause less constipation and nausea than do other opioids. | [17–19] |
| Codeine | Oral: 200 mg | Maximum of 360 mg/d. Used with or without acetaminophen. | [1,20] |
| Fentanyl | Transdermal: 12 µg/h × 24 h ~ 25 mg oral morphine/day. Transmucosal: no consensus; varies by product. | Delivered transdermally, transmucosally, or intravenously. Cachectic patients may have decreased absorption from transdermal patch. | [20–22] |
| Hydrocodone | Immediate release formulation with acetaminophen: 20 mg | Equianalgesic dose calculations for extended-release products vary; see prescribing information. | [1,23] |
| Hydromorphone | Oral: 6-7.5 mg, IV: 1.5 mg | [10,24] | |
| Methadone | Equianalgesic ratio varies widely by dose. | Used primarily for severe pain in non–opioid-naïve patients. Unusual pharmacokinetics require experienced practitioner. | [1,25,26] |
| Morphine | Oral: 30 mg, IV: 10 mg | Randomized trials supporting use. First-choice opioid because of familiarity, availability, and cost. | [1,20] |
| Oxycodone | 20 mg | Randomized trials supporting use. | [20] |
| Oxymorphone | 10 mg | [10] | |
| Tapentadol | 100 mg | Similar to morphine, 30-40 mg. | [24,27,28][Level of evidence: I] |
| Tramadol | 150 mg ~ 25 mg oral morphine | Use at <400 mg/d with or without acetaminophen. Used for moderate pain. Inhibits reuptake of norepinephrine and serotonin. Caution with concomitant antidepressant use. | [24] |
| Route | Agent | Comments | Reference(s) |
|---|---|---|---|
| NSAIDs = nonsteroidal anti-inflammatory drugs. | |||
| Buccal | Fentanyl | Used primarily for breakthrough pain. | [29] |
| Epidural | Opioids, local anesthetics | Consider if inadequate analgesia or intolerable side effects with oral or intravenous analgesics. | [1] |
| Intramuscular injection | Opioids, acetaminophen, ketorolac | Typically avoided because of pain from injection. | [10] |
| Intranasal | Fentanyl | Onset faster than that of transmucosal fentanyl or oral morphine. Used for breakthrough pain. | [29] |
| Intrathecal | Opioids | Consider if inadequate analgesia or intolerable side effects with oral or intravenous analgesics. | [1] |
| Intravenous | Most strong opioids (except oxycodone) and some NSAIDs | Availability varies by world region. | [10] |
| Oral | Most opioids except fentanyl and buprenorphine | Most common and preferred method of administration. | [10] |
| Rectal | Morphine, methadone | Onset similar to that of oral; possibly better absorption. May be useful for pediatric and end-of-life patients. | [1] |
| Subcutaneous | Morphine, fentanyl, hydromorphone, ketoprofen, methadone | Benefit similar to that of intravenous; considered an alternative if no oral capacity. | [1,2,30] |
| Sublingual | Fentanyl, buprenorphine, concentrated morphine solution, methadone | Used primarily for breakthrough pain. | [18,29] |
| Topical | Lidocaine | Primarily application of topical anesthetics. | [10] |
| Transdermal | Fentanyl, buprenorphine | Efficacy similar to that of oral agents for moderate to severe pain in opioid-naïve patients. | [1] |
| Transmucosal | Fentanyl | Used primarily for breakthrough pain. | [29] |
Rapid-onset fentanyl formulations
Rapid-onset opioids are developed to provide fast analgesia without using a parenteral route. Fentanyl, a synthetic opioid 50 to 100 times more potent than morphine, is available in a variety of delivery methods to offer additional options for management of breakthrough pain.[31] Along with rapid onset of action, these products avoid first-pass hepatic metabolism and intestinal digestion. For more information, see Table 4.
All rapid-acting fentanyl products are intended for use only in patients already tolerant to opioids and are not initiated in opioid-naïve patients. However, none are bioequivalent to others, making dose interchange complicated and requiring dose titration of each product individually, without regard to previous doses of another fentanyl product. The dose titration schedule is unique to each product, and it is critical that product information is reviewed individually when each product is used. The risk of addiction with these rapid-onset agents has not been elucidated. In the United States, prescription of these agents requires enrollment in the U.S. Food and Drug Administration’s (FDA’s) Risk Evaluation and Mitigation Strategies (REMS) program.
| Drug | Starting Dose (µg) | Tmax (median, minutes) | Comments | Evidence |
|---|---|---|---|---|
| DB = double blinded; PC = placebo controlled; RCT = randomized controlled trial; Tmax = time to maximum blood concentration. | ||||
| Transmucosal fentanyl lozenges (Actiq, generic) | 200 | 20–40 | Lozenge on stick, rubbed against cheek. Sugar content may increase dental caries. | Multiple RCTs showing benefit over placebo and oral morphine. |
| Fentanyl buccal tablet (Fentora) | 100, 200, or 400 | 35–45 | Absorption may be affected by mucositis. Before use, wet mouth if dry. | RCT showing benefit over placebo, and open-label study showing benefit for pain rescue; more rapid than oxycodone. |
| Fentanyl buccal film (Onsolis) | 200 | 60 | Before use, wet mouth if dry. | DB, PC, RCT showing benefit. |
| Fentanyl nasal spray (Lazanda) | 100 | 15–21 | Vial contains residual fentanyl when empty, requiring special disposal. Do not use with decongestant sprays. | DB, PC, RCT showed benefit. Open-label RCT showed benefit over transmucosal fentanyl and oral morphine. Most rapid onset. |
| Fentanyl sublingual spray (Subsys) | 100 | 40–75 | Contains residual fentanyl when empty, requiring special disposal. | Open-label and PC RCT showing benefit. |
| Fentanyl sublingual tablet (Abstral) | 100 | 30–60 | Absorption may be affected by mucositis. Before use, wet mouth if dry. | Multiple PC RCTs showing benefit. |
Methadone
Given the complexities related to methadone administration, it is important that this opioid be prescribed by experienced clinicians who can provide careful monitoring. Referral to a pain specialist or a palliative care team may be indicated.
Methadone is both a mu-receptor agonist and an N-methyl-D-aspartate (NMDA) receptor antagonist. It can be given via multiple routes (oral, intravenous, subcutaneous, and rectal); has a long half-life (13 to 58 hours) and rapid onset of action; and is inexpensive, making it an attractive option for cancer pain control. Because of its NMDA properties, methadone may be particularly useful for the management of opioid-induced neurotoxicity, hyperalgesia, and neuropathic pain, although further studies are needed to confirm these theoretical benefits. Methadone is safer than other opioids for patients with renal dysfunction, given that it is minimally renally excreted. It is preferred for those with known opioid allergies because it is a synthetic opioid. Additionally, it is long acting, whether given in crushed or liquid form, an important benefit when patients require drug administration via enteral tubes. However, methadone also has several distinct disadvantages, including drug interactions, the risk of QT prolongation, and a variable equianalgesic ratio, making rotation more challenging.
Methadone is metabolized by CYP2B6, CYP2C19, CYP3A4, and CYP2D6. The principal enzyme responsible for methadone levels and drug clearance is CYP2B6.[32] CYP3A4 inducers (e.g., certain anticonvulsants and antiretroviral agents) can potentially reduce its analgesic effect.[33] In contrast, enzyme inhibitors may increase methadone’s activity, including side effects. For clinicians, the potential for significant drug-drug interactions may mean that some medications need to be replaced and that patients need extra monitoring. Furthermore, because methadone is a substrate of P-glycoprotein, medications that inhibit the activity of this transporter, such as verapamil and quinidine, may increase methadone’s bioavailability.
Methadone is associated with QT prolongation. This risk increases in patients receiving high doses (especially >100 mg/day) or with preexisting risk factors, including treatment with some anticancer agents. For patients with risk factors for QT prolongation, it is important to conduct a baseline electrocardiogram (ECG) before treatment with methadone. A follow-up ECG is recommended at 2 to 4 weeks after methadone initiation if the patient has known risk factors, with the occurrence of new risk factor(s) for all patients, and when the doses of methadone reach 30 to 40 mg/day and 100 mg/day for all patients regardless of risk, if consistent with goals of care.[32,34]
Because the equianalgesic ratio between methadone and other opioids is unpredictable, most health care professionals recommend starting at a low dose twice daily, with gradual dose escalation every 3 to 5 days or at longer intervals.[32] Short-acting opioids, not methadone, should also be available for breakthrough pain. References further describe switching from opioids to methadone.[25,26]
A systematic review has highlighted three approaches to methadone conversion in the literature.[35,36] However, the quality of the evidence was low, making it difficult to conclude which approach was superior. Rapid titration of methadone may result in delayed respiratory depression because of its long half-life.[37]
Adverse effects
Adverse effects from opioids are common and may interfere with achieving adequate pain control (see Table 5). However, not all adverse effects are caused by opioids, and other etiologies also need to be evaluated. Examples of relevant factors include the following:[38]
- Symptoms from disease progression.
- Comorbid health conditions.
- Drug interactions (including adjuvant analgesics).
- Clinical conditions such as dehydration or malnutrition.
In general, options for addressing adverse effects associated with opioids include aggressive management of the adverse effects, opioid rotation, or dose reduction. In most instances, definitive recommendations are not possible.
| Adverse Effect | Relative Prevalenceb | Comments | |
|---|---|---|---|
| Acute Usec | Chronic Used | ||
| aThe reported prevalence may differ on the basis of opioid choice, dose, route, and duration of use. | |||
| bRelative prevalence: (–) absent; (+) rare; (++) less common; (+++) common. | |||
| cAcute use defined as use for ≤2 weeks, as-needed use, and upon significant dose increase. | |||
| dChronic use defined as consistent use for >2–3 months at stable doses. | |||
| Cardiovascular | |||
| Hypotension | + | + | Mostly with intravenous opioids. |
| Central nervous system | |||
| Sedation | +++ | + | More common upon opioid initiation and dose increase.[39] |
| Dizziness | ++ | + | [10] |
| Delirium/hallucinations | + | + | [10] |
| Impaired cognitive status | ++ | + | [10] |
| Sleep disturbances | ++ | + | [10] |
| Gastrointestinal | |||
| Nausea | +++ | + | Slow upward dose titration reduces risk. Lower rates with hydromorphone vs. morphine.[39,40] |
| Vomiting | ++ | + | [10] |
| Constipation | +++ | +++ | [41] |
| Autonomic nervous system | |||
| Xerostomia | +++ | + | [10] |
| Bladder dysfunction/urinary retention | + | + | [10] |
| Respiratory | |||
| Respiratory depression | + | – | Extremely rare if used appropriately.[39] |
| Dermatologic | |||
| Pruritus | ++ | – | More common with spinal analgesia.[39] |
| Miscellaneous | |||
| Hyperalgesia | – | + | Observed more commonly with opioid-induced neurotoxicity. May be more common with morphine and hydromorphone.[42] |
| Opioid endocrinopathy/hypogonadism | – | + | [43,44] |
| Hypoglycemia | + | + | May be observed among patients on tramadol or methadone. More common among diabetics. |
Opioid-induced neurotoxicity (OIN)
OIN is a broad term used to encompass the neuropsychiatric effects that result from opioid use, including:
- Sedation.
- Hallucinations.
- Delirium.
- Myoclonus.
- Seizures.
- Hyperalgesia.
The mechanism behind OIN may be attributed to opioids’ anticholinergic activity, endocytosis of opioid receptors, and stimulation of N-methyl-D-aspartate receptors.[45,46] Patients are at increased risk of OIN if they are receiving an opioid with active metabolites such as morphine or codeine, are older adults, have renal dysfunction or active infection, or are dehydrated. A retrospective study was conducted in patients with advanced cancer who received palliative care consultations at the University of Texas MD Anderson Cancer Center; the researchers sought to determine the frequency of and risk factors for OIN in 390 patients who had been taking opioids for 24 hours or longer.[47] A board-certified palliative care specialist diagnosed OIN using the Edmonton Symptom Assessment Scale and the Memorial Delirium Assessment Scale. Symptoms were attributed to OIN if a patient had no past medical history of that symptom; the differential diagnosis of other causes was excluded; and/or the symptoms improved upon discontinuation, decrease, or change in opioid dose. The authors found that 15% of the patients developed at least one symptom of OIN, the most common of which was delirium (47%). The mean morphine equivalent daily dose was 106 mg in patients without OIN and 181 mg in patients with OIN. Sedation and drowsiness were common but typically transient adverse effects.
Patients who have persistent problems may benefit from opioid rotation. Methylphenidate has been proposed as an intervention to reduce opioid-induced sedation.[48,49] The effects of opioids on cognitive or psychomotor functioning are not well established. Given the incidence of sedation, caution is exercised when an opioid is initiated or when dose escalation is required. There is less evidence, however, that patients on chronic stable doses exhibit cognitive or motor impairment.[50]
Delirium is associated with opioids but is typically multifactorial in origin.[51] In one retrospective study, 80% of the delirium cases were not related to opioids.[52] For more information about managing delirium, see the Delirium section in Last Days of Life.
Hyperalgesia
In contrast to opioid tolerance, opioid-induced hyperalgesia (OIH) occurs when a patient who has been taking opioids long-term experiences paradoxical pain in regions unaffected by the original pain complaint.[42,53–56] This paradoxical pain often results in clinicians increasing doses of pain medications. OIH is also defined as “the need for increasingly high levels of opioids to maintain pain inhibition after repeated drug exposure.” OIH is a clinical phenomenon that has been differentiated from opioid tolerance in the research literature in a mouse model.[54]
The clinical relevance needs to be further studied, and this issue may be underappreciated in clinical practice.
A thorough history and physical are appropriate if OIH is suspected. Changes in pain perception and increasing opioid requirements may be caused by OIH, opioid tolerance, or disease progression. There is no standard recommendation for the diagnosis and treatment of OIH. A trial of incremental opioid dose reductions may lead to an improvement in pain from OIH. However, this may be psychologically distressing to oncology patients who require opioid treatment. Opioid rotation is a strategy frequently employed if opioid tolerance has occurred. Methadone is an ideal opioid to switch to, given its mechanism of action as an opioid receptor agonist and NMDA receptor antagonist. Given the similarities between OIH and neuropathic pain, the addition of an adjunctive medication such as pregabalin has been recommended.[42]
Respiratory depression
Opioid-induced respiratory depression may be caused by a blunting of the chemoreceptive response to carbon dioxide and oxygen levels and altered mechanical function of the lung necessary for efficient ventilation and gas exchange.[57] Opioid-induced respiratory depression may manifest through decreased respiratory rate, hypoxemia, or increases in total exhaled carbon dioxide.[58] The prevalence of respiratory depression is not known but rarely occurs with proper opioid use and titration.[59–62] The following factors contribute to opioid-induced respiratory depression:
- Obstructive sleep apnea.
- Obesity.
- Concomitant sedating medications.
If respiratory depression is thought to be related to opioids (e.g., in conjunction with pinpoint pupils and sedation), naloxone, a nonselective competitive opioid antagonist, may be useful. However, careful titration should be considered because it may compromise pain control and may precipitate withdrawal in opioid-dependent individuals. Because of methadone’s long half-life, naloxone infusion may be required for respiratory depression caused by methadone. For patients receiving opioids at home, nasal naloxone is indicated, particularly for those at greatest risk of respiratory depression, or if there is a concern about misuse or accidental use by others in the household.
Nausea and vomiting
Opioid-induced nausea occurs in up to two-thirds of patients receiving opioids, and half of those patients will experience vomiting.[63] Opioids cause nausea and vomiting via enhanced vestibular sensitivity, via direct effects on the chemoreceptor trigger zone, and by causing delayed gastric emptying.[64] Antiemetics may be started up front in patients at risk of developing nausea, or instituted once symptoms occur. Tolerance to opioid-induced nausea and vomiting (OINV) may develop, and symptoms should resolve within 1 week. If symptoms persist despite treatment with antiemetics, opioid rotation can be considered, or other causes of nausea can be investigated.
OINV is treated with many of the same antiemetic drugs that are used for chemotherapy-induced nausea and vomiting. Although many antiemetic regimens have been proposed for OINV, there is no current standard.[64] The chemoreceptor trigger zone is stimulated by dopamine, serotonin, and histamine. Metoclopramide may be a particularly attractive option because of its dual antiemetic and prokinetic effects. Other dopamine antagonists such as prochlorperazine, promethazine, and olanzapine have been used to treat OINV. For patients whose nausea worsens with positional changes, a scopolamine patch has been found effective. Serotonin antagonists such as ondansetron may be used. However, they could worsen constipation among patients already taking opioids.
Constipation
Constipation is the most common adverse effect of opioid treatment, occurring in 40% to 95% of patients.[65] It can develop after a single dose of morphine, and patients generally do not develop tolerance to opioid-induced constipation. Chronic constipation can result in hemorrhoid formation, rectal pain, bowel obstruction, and fecal impaction.
Opioids cause constipation by decreasing peristalsis, which occurs by reducing gastric secretions and relaxing longitudinal muscle contractions, and results in dry, hardened stool.[66] Constipation is exacerbated by dehydration, inactivity, and comorbid conditions such as spinal cord compression. Patients are encouraged to maintain adequate hydration, increase dietary fiber intake, and exercise regularly, in addition to taking laxatives.
A scheduled stimulant laxative, such as senna, is started with opioid initiation. The addition of a stool softener offers no further benefit.[67,68] Laxatives are titrated to a goal of one unforced bowel movement every 1 to 2 days. If constipation persists despite prophylactic measures, then additional assessment of the cause and severity of constipation is performed. After obstruction and impaction are ruled out, other causes of constipation (such as hypercalcemia) are treated.
There is no evidence to recommend one laxative class over another in this setting. Appropriate drugs include the following:
- Bisacodyl.
- Polyethylene glycol.
- Magnesium hydroxide.
- Lactulose.
- Sorbitol.
- Magnesium citrate.
Suppositories and enemas are generally avoided in the setting of neutropenia or thrombocytopenia.
Methylnaltrexone and naloxegol are peripherally acting opioid antagonists approved for the treatment of opioid-induced constipation in patients who have had inadequate response to conventional laxative regimens. Laxatives are discontinued before peripherally acting opioid antagonists are initiated. These agents are not used if postoperative ileus or mechanical bowel obstruction is suspected.[69,70]
Of note, several combination opioid and opioid-antagonist products (e.g., oxycodone-naltrexone) are FDA approved for pain management and have the added benefit of potentially preventing opioid-induced constipation.[71] Given the limited data about these agents in cancer patients and the high cost of these agents, further data are needed.
Opioid endocrinopathy
Opioid endocrinopathy (OE) is the effect of opioids on the hypothalamic-pituitary-adrenal axis and the hypothalamic-pituitary-gonadal axis over the long term. Opioids act on opioid receptors in the hypothalamus, decreasing the release of gonadotropin-releasing hormone.[72] This results in a decreased release of luteinizing hormone and follicle-stimulating hormone, and finally a reduction of testosterone and estradiol released from the gonads. These effects occur in both men and women.[44] Patients may present with the following symptoms of hypogonadism:
- Decreased libido.
- Erectile dysfunction.
- Amenorrhea or irregular menses.
- Galactorrhea.
- Depression.
- Hot flashes.
Treatment for OE is not well established. One group of investigators performed a 24-week, open-label pilot study of a testosterone patch in 23 men with opioid-induced androgen deficiency and reported an improvement in androgen deficiency symptoms, sexual function, mood, depression, and hematocrit levels.[73] There was no change in opioid use. Men and women with OE may be offered hormone replacement therapy after a thorough risk-benefit discussion. Testosterone replacement is contraindicated in men with prostate cancer; estrogen replacement therapy may be contraindicated in patients with breast and ovarian cancer and has serious associated health risks.
Opioid-induced immunological changes
Opioids have immunomodulatory effects through neuroendocrine mechanisms and by direct effects on opioid receptors on immune cells.[74] Opioids can alter the development, differentiation, and function of immune cells, causing immunosuppression.[43] Different opioids cause varying effects on the immune system. In mouse and rat models, methadone is less immunosuppressive than morphine. In contrast, tramadol improves natural killer cell activity. Further research is needed to determine the true clinical significance of opioid-induced immunosuppression, such as the risk of infections.
Liver disease
The liver plays a major role in the metabolism and pharmacokinetics of opioids and most drugs. The liver produces enzymes involved in two forms of metabolism:[33]
- Phase 1 metabolism (modification reactions, CYP).
- Phase 2 metabolism (conjugation reactions, glucuronidation).
Methadone and fentanyl are unaffected by liver disease and are drugs of choice in patients with hepatic failure.[75,76]
Morphine, oxymorphone, and hydromorphone undergo glucuronidation exclusively. CYP2D6 metabolizes codeine, hydrocodone, and oxycodone; CYP3A4 and CYP2D6 metabolize methadone; and CYP3A4 metabolizes fentanyl.[33] Hepatic impairment affects both CYP enzymes and glucuronidation processes. Prescribing information recommends caution when prescribing opioids for patients with hepatic impairment.
In cirrhosis, the elimination half-life and peak concentrations of morphine are increased.[77] Moderate to severe liver disease increases peak levels and the area under the curve (AUC) for both oxycodone and its chief metabolite, noroxycodone.[78] Peak plasma concentrations and AUC of another active metabolite, oxymorphone, are decreased by 30% and 40%, respectively.[78]
Although oxymorphone itself does not undergo CYP-mediated metabolism, a portion of the oxycodone dose is metabolized to oxymorphone by CYP2D6. Failure to convert oxycodone to oxymorphone may result in accumulation of oxycodone and noroxycodone, with an associated increase in adverse events. Hepatic disease increases the bioavailability of oxymorphone as liver function worsens.[79]
Renal insufficiency
Renal insufficiency affects the excretion of morphine, codeine, oxycodone, hydromorphone, oxymorphone, and hydrocodone. Methadone and fentanyl are safe to use in patients with renal failure, although there is some evidence that the hepatic extraction of fentanyl is affected by uremia.[80]
When patients with renal insufficiency receive hydromorphone and morphine, both hydromorphone and morphine metabolites accumulate, with the potential to cause neuro-excitatory adverse effects. Morphine, which has a higher risk of drug and metabolite accumulation, may be used in patients with mild renal failure but requires dosing at less-frequent intervals or at a lower daily dose to provide benefit with adequate safety.[78] In patients with stage III to stage IV chronic kidney disease (glomerular filtration rate <59 mL/min), morphine may not be desirable.[78]
There are conflicting reports about the safety of hydromorphone in patients with renal failure. One case series suggests adverse effects increasing when hydromorphone is given by continuous infusion to patients with renal failure.[81] Other series suggest that it is safe to use.[82] Although renal impairment affects oxycodone more than it does morphine, there is no critical accumulation of an active metabolite that produces adverse events.[78]
Opioid rotation
Opioid rotation or switching may be needed when one of the following situations occurs:[83,84]
- The patient is experiencing side effects beyond what can be managed with simple measures. For example, the presence of OIN (e.g., sedation, hallucinations, delirium, myoclonus, seizures, or hyperalgesia) almost always warrants opioid rotation.
- Pain control remains suboptimal despite an active effort to titrate the opioid dose. Ideally, the patient’s opioid dose is increased to the highest tolerable level before switching occurs to avoid abandoning an opioid prematurely.
- A switch is needed for logistical reasons, such as change in the route of administration (e.g., from intravenous to oral in preparation for discharge or from oral to transdermal due to severe odynophagia); the need to minimize toxicities after the onset of renal/hepatic failure (e.g., from morphine to fentanyl or methadone); and cost considerations (e.g., from long-acting oxycodone to methadone).
The selection of a target opioid depends on the reason for rotation. All strong opioids have similar efficacy and side-effect profiles at equianalgesic doses. Because of the lack of predictors for specific opioids, empirical trials are needed to identify the ideal opioid for a patient. If OIN is the reason for switching, it may not matter which opioid is switched to, as long as it is a different agent. Patient preference, history of opioid use, route of administration, and cost are necessary considerations before the final choice is made.
A study of opioid rotation in the outpatient palliative care setting revealed that approximately one-third of 385 consecutive patients needed an opioid rotation, mostly for uncontrolled pain (83%) and OIN (12%).[85] The success rate was 65%, with a median pain improvement of two points out of ten (minimal clinically important difference is one point).[86]
Barriers related to opioid use
The barriers to appropriate use of opioids in the treatment of cancer pain include misunderstanding or misapprehension about opioids by health care providers, patients, and society. One group of investigators surveyed 93 patients with cancer cared for in an academic practice in Australia to understand patient-level concerns about the use of opioids.[87] One-third of the patients reported high levels of pain that adversely affected activity, mood, sleep, and enjoyment of life. High percentages of patients reported concerns about addiction (76%) or side effects (67%). In addition, patients expressed concerns that the pain represented disease progression (71%), that they were distracting the doctor (49%), or that they would not be seen as a “good patient” (46%).[87] Patients with more severe pain were more likely to express concerns about side effects and were less likely to use unconventional approaches to control pain. Results were similar to those of a survey of American patients from the previous decade.[88]
Physician-perceived barriers to opioid prescribing tend to parallel those of patients.[89] For example, physicians and other health care providers have beliefs about addiction that inhibit prescribing. For some, these beliefs are informed by guidelines and data extrapolated from a noncancer population. Guidelines influence physician prescribing and, at times, may be applied to populations who are not addressed in a guideline. For instance, after the Centers for Disease Control and Prevention (CDC) updated its guideline on prescribing opioids for chronic noncancer pain in 2016, [90] the mean number of opioids prescribed by oncologists per 100 Medicare beneficiaries decreased by 22.2%, from 69.0 in 2013 to 53.7 in 2017. This effect was widespread, with decreased prescribing noted in 43 of 50 U.S. states.[91] These changes in prescribing patterns resulted in decreases in frequency, dose, and duration of opioid prescriptions for U.S. patients with cancer-related pain.[92] In a large study of Medicare patients with poor prognoses, a decrease in opioid prescribing from 2007 to 2017 was correlated with an increase in emergency department visits near the end of life. This finding raises concerns about undertreated pain in this population.[93]
Similarly, a cohort study in a pediatric population compared opioid prescription rates for 8,969 privately insured pediatric cancer survivors who were 1 year off therapy (aged ≤21 years at diagnosis) and 44,845 matched peers without cancer during the time before (7 years) and after (2 years) the CDC opioid prescribing guideline. Indicators for potential misuse were 1) high daily opioid dose (≥100 MMEs daily), 2) multiple opioid prescription overlap of 7 days or more, 3) opioid and benzodiazepine overlap of 7 days or more, or 4) opioid dose escalation (≥50% increase in monthly average MME twice per year). Relative reduction in opioid prescription rates were 36.7% in survivors versus 15.9% in peers without cancer. Relative reduction in the rate of potential misuse and substance use disorder was 65.4% in survivors and 29.9% in peers without cancer. These findings raise concerns that the guideline affected access to opioid-based strategies for pain control for pediatric patients with cancer and during survivorship.[94]
Racial inequities are also seen in opioid prescribing. They worsened between 2007 and 2019 and disproportionately affected Black men. A study evaluated 318,549 non-Hispanic White, Black, and Hispanic Medicare-covered decedents older than 65 years with poor-prognosis cancers. It demonstrated that Black and Hispanic patients were less likely to receive any opioid (Black, -4.3 percentage points, 95% Confidence Interval (CI), -4.8 to -3.6; Hispanic, -3.6 percentage points, 95% CI, -4.4 to -2.9), received lower daily doses (Black, -10.5 MMEs per day [MMED], 95% CI, -12.8 to -8.2; Hispanic, -9.1 MMED, 95% CI, -12.1 to -6.1), and lower total doses (Black, -210 MMEs, 95% CI, -293 to -207; Hispanic, -179 MMEs, 95% CI, -217 to -142). Black patients were also more likely to undergo urine drug screening (0.5 percentage points; 95% CI, 0.3–0.8). Adjustment for socioeconomic factors did not attenuate the end-of-life opioid access disparities.[95] In a study that evaluated patients with head and neck cancer who received care from 2017 to 2021, White patients were significantly more likely than non-White patients to receive a new prescription for pain (adjusted odds ratio [OR], 2.52; 95% CI, 1.09–5.86), despite no statistically significant difference in odds of pain reporting between the groups (adjusted OR, 0.97; 95% CI, 0.73–1.30).[96][Level of evidence: III]
Many states have developed prescription drug monitoring programs, and the FDA requires REMS (a risk evaluation and management strategy) for certain opioids, such as rapid-onset fentanyl products. These requirements could be an additional barrier to opioid prescribing. Other barriers include poor or limited formulary and reimbursement for opioids.
Opioids and risk of addiction
In the United States, the number of deaths from opioid overdose in 2019 was nearly 50,000, over six times greater than in 1999.[97] In 2013 alone, 2 million Americans were estimated to have either abused or been dependent on opioids, with 22,767 deaths related to prescription drug overdose. Although most cancer patients prescribed opioids are using them safely, one study estimated that up to 8% of cancer patients may be addicted to opioids.[98] Thus, it is important for clinicians treating cancer patients for pain to provide careful monitoring and to adopt safe opioid-prescribing practices.[99]
To characterize opioid use disorder (OUD) and overdose in cancer patients, a retrospective cohort study was conducted using 2007 to 2014 Surveillance, Epidemiology, and End Results (SEER) Program–Medicare data for patients with a diagnosis of stage 0 to stage III breast, prostate, or colon cancer.[100] Patients with cancer were paired with up to two matched control patients without cancer. OUD and overdose were defined using Chronic Conditions Warehouse claims–based algorithms. These algorithms included, for example, ICD-9 codes for opioid-type dependence, opioid abuse, and poisonings by opiates and related narcotics. The unadjusted rates of composite OUD and nonfatal overdose were 25.2, 27.1, 38.9, and 12.4 events per 10,000 patients in the noncancer, breast cancer, colorectal cancer, and prostate cancer groups, respectively. There was no association between cancer and OUD. Interestingly, when opioid overdose was analyzed separately from OUD, colorectal cancer survivors had 2.33 times higher odds of opioid overdose in the 12 months after cancer diagnosis, compared with matched controls.
Most patients begin opioid therapy after an acute event such as a pain crisis from cancer progression or surgery.[101] Sometimes cancer treatment and its effects will lead to increased opioid use, with approximately 10% of patients continuing to take the equivalent of 30 mg of hydrocodone per day at 1 year post–curative surgery.[102] All patients taking opioids require assessment for risk of abuse or addiction.[101] For more information, see Table 6.
Addiction is defined as continued, compulsive use of a drug despite harm. Many other conditions may be misidentified as addiction, and it is important that clinicians distinguish between the two.[103] These conditions include the following:[104,105]
- Aberrant behavior: A behavior outside the boundaries of the agreed-on treatment plan that is established as early as possible in the doctor-patient relationship.[106]
- Chemical coping: The use of opioids to cope with emotional distress, characterized by inappropriate and/or excessive opioid use.[105]
- Diversion: Redirection of a prescription drug from its intended user to another individual.
- Misuse: Inappropriate use of a drug, whether deliberate or unintentional.
- Physical dependence: Condition in which abrupt termination of drug use causes withdrawal syndrome.
- Pseudo-addiction: Condition characterized by behaviors such as drug hoarding that mimic addiction but are driven by a desire for pain relief; usually signals undertreated pain or anxiety that future pain will be untreated.
- Self-medication: Use of a drug without consulting a health care professional to alleviate stressors or disorders such as depression or anxiety.
- Substance use disorder: Maladaptive pattern of substance use leading to considerable impairment or distress.
- Tolerance: Phenomenon in which analgesia decreases as the body grows tolerant to a given dosage of a drug, requiring an increased dose to achieve the same analgesic effect.[104]
The following aberrant behaviors may suggest addiction or abuse; further assessment is required to make the diagnosis:
- Aggressive complaining about the need for more drugs.
- Drug hoarding during periods of reduced symptoms.
- Acquiring similar drugs from other medical sources.
- Requesting specific drugs.
- Reporting psychic effects not intended by the physician.
- Resistance to a change in therapy associated with tolerable adverse effects accompanied by expressions of anxiety related to the return of severe symptoms.
- Resistance to referral to a mental health professional.
- Unapproved use of the drug to treat another symptom or use of the drug for a minor symptom (e.g., use of fentanyl for mild headache pain).
- Unsanctioned dose escalation or other nonadherence to therapy on one or two occasions.
- Unconfirmed multiple allergies to multiple opioids.
| Tool | Description | Comments |
|---|---|---|
| aAdapted from DiScala SL, Lesé MD: Chronic pain. In Murphy JE, Lee MW, eds.: Pharmacotherapy Self-Assessment Program. Book 2: CNS/Pharmacy Practice. Lenexa, Kan: American College of Clinical Pharmacy, 2015, p. 102. | ||
| Current Opioid Misuse Measure (COMM) | 17-item self-assessment tool for patients | Identifies aberrant behaviors; for those with chronic pain who are already on opioids. |
| Diagnosis, Intractability, Risk, Efficacy (DIRE) | 8-item tool | Determines risk of long-term opioid use in those with chronic pain; evaluates regimen efficacy. |
| Opioid Risk Tool (ORT) | 5-item tool | Predicts aberrant or drug-related behaviors. |
| Prescription Drug Use Questionnaire (Self-Report) (PDUQp) | 31-item self-assessment tool | Evaluates and predicts opioid misuse in those with chronic pain. |
| Pain Medication Questionnaire (PMQ) | 26-item tool | Evaluates risk of opioid misuse in those with chronic pain. |
| Screening Instrument for Substance Abuse Potential (SISAP) | 5-item tool | Evaluates those with history of substance use disorder and risk of opioid misuse; used in primary care setting. |
| Screener and Opioid Assessment for Patients with Pain (SOAPP) Version 1.0 | 24-item self-assessment | Evaluates risk of long-term opioid therapy in those with chronic pain. |
| Screener and Opioid Assessment for Patients with Pain—Revised (SOAPP-R) | 24-item self-assessment | Evaluates those already taking opioids, or those about to begin (before initiation of therapy). |
Risk factors for opioid abuse include the following:[103]
- Smoking.
- Psychiatric disorders.
- History of childhood sexual abuse.
- Personal or family history of substance use disorder.
Screening tools help in risk assessment. Common tools include the following:
The choice of which tool to use depends on the type of practice. The ORT is short and useful for busy practices.[104] None of the screening tools have been validated in an oncology population.
Risk assessment determines the structure of therapy, which can range from minimal structure to more structure.[110] Highly structured opioid therapy requires the following approaches:[103]
- Frequent visits.
- Limit on number of pills per prescription.
- Use of other specialists.
- Use of urine drug testing.
Opioid agreements outline what is expected of the patient, educate about drug storage, and delineate acceptable and unacceptable behavior.[111] Patients are taught that they must safeguard their medications “like their wallets” to protect against diversion. In addition, state guidelines for chronic opioid use, state prescription monitoring, and the use of pharmacists may reduce the potential for worsening addictive behavior.[112]
Random urine drug testing is used for patients with an inadequate response to opioid therapy and those receiving opioids long term as part of a risk mitigation strategy.[113] A urine drug test demonstrating absence of prescribed opioid can be useful because it suggests either diversion or stockpiling; a urine drug test revealing concurrent use of other nonprescribed medications or illicit substances can also be informative. Because many different types of urine drug tests are available, clinicians may want to become familiar with the types and interpretation of tests available locally. Awareness of false-positive and false-negative results is crucial to accurate interpretation.[114] A clinician’s laboratory can identify the substance in question. Clinicians use urine drug testing differently, with some requiring it at the initiation of therapy, episodically, or at the transition to long-term opioid therapy. Risk assessment helps to determine frequency of urine drug testing.[113]
Pharmacological deterrence has emerged as another option designed to dissuade misuse and abuse by making it difficult to obtain euphoric effects from opioid use.[113] Creating barriers to increasing the bioavailability of opioids is one method of pharmacological deterrence. One approach is to add an opioid antagonist to the formulation.[115] Embedding opioid into a matrix that cannot be obtained by crushing or chemical extraction is another pharmacological deterrent.[116]
Adjuvant Pain Medications
Gabapentin and pregabalin
Gabapentin and pregabalin are structurally related to the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) but have no effect on GABA binding. Instead, they bind to the alpha2delta-1 subunit of voltage-gated calcium channels, which may result in decreased neuronal excitability in pain-associated sensory neurons. These drugs have been widely studied in the treatment of neuropathic pain syndromes and as adjunctive agents with opioids. For more information, see the Approach to Neuropathic Pain section.
These medications may cause the following symptoms:[10,117]
- Sedation.
- Dizziness.
- Peripheral edema.
- Nausea.
- Ataxia.
- Dry mouth.
Gradual upward titration of gabapentin to a maximum of 3,600 mg per day and pregabalin to 300 mg per day can help with dose-dependent sedation and dizziness. In addition, starting doses of gabapentin may be given at bedtime to assist with tolerating any sedation. Doses of both agents need to be adjusted for patients with renal dysfunction.[10,117]
Venlafaxine and duloxetine
The antidepressant medications venlafaxine and duloxetine have demonstrated some efficacy in the treatment of neuropathic pain syndromes. Venlafaxine and duloxetine are serotonin and norepinephrine reuptake inhibitors (SNRIs) originally approved for depression; however, both are used off-label for the treatment of chemotherapy-induced peripheral neuropathy (CIPN). In addition, duloxetine is indicated for musculoskeletal pain. Both serotonin and norepinephrine have important roles in analgesia.
Common dosing for duloxetine ranges from 30 mg to 60 mg per day. Side effects include the following:[118]
- Nausea.
- Headache.
- Fatigue.
- Dry mouth.
- Constipation.
Duloxetine is avoided in patients with hepatic impairment and severe renal impairment, and it carries an increased risk of bleeding.
Venlafaxine inhibits serotonin reuptake more intensely at low doses, and norepinephrine more intensely at higher doses; higher doses may be necessary for relief of CIPN.[119]
Venlafaxine can be started at 37.5 mg, with a maximum dose of 225 mg per day. Adverse effects include nausea, vomiting, headache, somnolence, and hypertension at higher doses. These effects decrease with the use of the long-acting formulations. Venlafaxine is used with caution in patients with bipolar disorder or a history of seizures and is dose-adjusted for patients with renal or hepatic insufficiency. If the decision is made to discontinue either venlafaxine or duloxetine, a slow tapering course may help to minimize withdrawal symptoms.
Tricyclic antidepressants (TCAs)
The TCAs amitriptyline, desipramine, and nortriptyline are used to treat many neuropathic pain syndromes. These drugs enhance pain inhibitory pathways by blocking serotonin and norepinephrine reuptake.
TCAs have anticholinergic, antihistaminic, and antiadrenergic effects that result in the following:
- Dry mouth.
- Drowsiness.
- Weight gain.
- Orthostatic hypotension.
Significant drug interactions are a concern, including interactions with anticholinergics, psychoactive medications, class IC antiarrhythmics, and selective serotonin reuptake inhibitors (SSRIs). Because of these adverse effects and drug interactions, TCAs are used with caution in older patients, patients with seizure disorders, and those with preexisting cardiac disease.
Corticosteroids
There is a lack of high-quality data demonstrating the efficacy of corticosteroids in treating cancer pain. A systematic review of the literature resulted in four randomized controlled trials and concluded that there is low-grade evidence to suggest corticosteroids have moderate activity in the treatment of cancer pain.[120] A small but well-designed study showed no benefit to adding corticosteroids to opioid analgesia in the short term (7 days).[121]
Despite the lack of good evidence, corticosteroids are often used in the clinical setting. Corticosteroids (dexamethasone, methylprednisolone, and prednisone) may be used as adjuvant analgesics for cancer pain originating in bone, neuropathy, and malignant intestinal obstruction. Mechanisms of analgesic action include decreased inflammation, decreased peritumoral edema, and modulation of neural activity and plasticity.[122]
Although there is no established corticosteroid dose in this setting, recommendations range from a trial of low-dose therapy such as dexamethasone 1 mg to 2 mg or prednisone 5 mg to 10 mg once or twice daily,[123] to dexamethasone 10 mg twice daily.[124] A randomized trial demonstrated that dexamethasone (8 mg on day of radiation therapy and daily for the following 4 days) reduces the incidence of pain flares, compared with placebo.[125] For more information, see the External-Beam Radiation Therapy section.
The immediate side effects of corticosteroid use include:
- Hyperglycemia.
- Insomnia.
- Immunosuppression.
- Psychiatric disorders.
Serious long-term effects—myopathy, peptic ulceration, osteoporosis, and Cushing syndrome—encourage short-term use of corticosteroids. If taken for more than 3 weeks, corticosteroids are tapered upon improvement in pain, if possible. If corticosteroids are to be continued long term, anti-infective prophylaxis can be considered. Dexamethasone is preferred because it has reduced mineralocorticoid effects, resulting in reduced fluid retention; however, it does exhibit cytochrome P450–mediated drug interactions.
Bisphosphonates and denosumab
The bisphosphonate class of drugs inhibits osteoclastic bone resorption, decreasing bone pain and skeletal-related events associated with cancer that has metastasized to the bone. Pamidronate and zoledronic acid decrease cancer-related bone pain, decrease analgesic use, and improve quality of life in patients with bone metastases.[126–129] American Society of Clinical Oncology (ASCO) guidelines for the use of these bone-modifying agents in patients with breast cancer and myeloma specify they should be used not as monotherapy but as part of a treatment regimen that includes analgesics and nonpharmacological interventions.[130,131] Bisphosphonates can cause an acute phase reaction characterized by fever, flu-like symptoms, arthralgia, and myalgia that may last for up to 3 days after administration. Additional adverse effects include renal toxicity, electrolyte imbalances, and osteonecrosis of the jaw.[132–134] Doses are adjusted for patients with renal dysfunction.
A single dose of ibandronate 6 mg was compared with a single fraction of radiation for localized metastatic bone pain in 470 prostate cancer patients.[135] Patients were allowed to cross over if they failed to respond at 4 weeks. Pain was assessed at 4, 8, 12, 26, and 52 weeks. Pain response was not statistically different between the two groups at 4 or 12 weeks; however, a faster onset of pain response was seen in the radiation therapy group. Interestingly, patients who crossed over and received both treatments had a longer overall survival than did patients who did not cross over. The authors concluded that ibandronate provides a feasible alternative to radiation therapy for the treatment of metastatic bone pain when radiation therapy is not an option.
Denosumab is a fully human monoclonal antibody that inhibits the receptor activator of nuclear factor kappa beta ligand (RANKL), prevents osteoclast precursor activation, and is primarily used in the treatment of bone metastases. A review of six trials comparing zoledronic acid with denosumab demonstrated a greater delay in time to worsening pain for denosumab (relative risk, 0.84; 95% CI, 0.77–0.91).[136]
Compared with zoledronic acid, denosumab has similar adverse effects with less nephrotoxicity and increased hypocalcemia. There is no adjustment for renal dysfunction; however, patients with a creatinine clearance lower than 30 mL/min are at a higher risk of developing hypocalcemia. Denosumab may be more convenient than zoledronic acid because it is a subcutaneous injection and not an intravenous infusion; however, it is significantly less cost-effective.[137]
Ketamine
Ketamine is an FDA-approved dissociative general anesthetic that has been used off-label in subanesthetic doses to treat opioid-refractory cancer pain. A 2012 Cochrane review of ketamine used as an adjuvant to opioids in the treatment of cancer pain concluded there is insufficient evidence to evaluate its efficacy in this setting.[138]
Lack of demonstrated clinical benefit, significant adverse events, and CYP3A4-associated drug interactions limit ketamine’s utility in the treatment of cancer pain. It is an NMDA receptor antagonist that, at low doses, produces analgesia, modulates central sensitization, and circumvents opioid tolerance. However, a randomized placebo-controlled trial of subcutaneous ketamine in patients with chronic uncontrolled cancer pain failed to show a net clinical benefit when ketamine was added to the patients’ opioid regimen.[139] Adverse drug reactions include the following:
- Hypertension.
- Tachycardia.
- Psychotomimetic effects.
- Increased intracranial and intraocular pressure.
- Sedation.
- Delirium.
- Impaired bladder function.
Current Clinical Trials
Use our advanced clinical trial search to find NCI-supported cancer clinical trials that are now enrolling patients. The search can be narrowed by location of the trial, type of treatment, name of the drug, and other criteria. General information about clinical trials is also available.
References
- Caraceni A, Hanks G, Kaasa S, et al.: Use of opioid analgesics in the treatment of cancer pain: evidence-based recommendations from the EAPC. Lancet Oncol 13 (2): e58-68, 2012. [PUBMED Abstract]
- Mercadante S, Giarratano A: The long and winding road of non steroidal antinflammatory drugs and paracetamol in cancer pain management: a critical review. Crit Rev Oncol Hematol 87 (2): 140-5, 2013. [PUBMED Abstract]
- Stockler M, Vardy J, Pillai A, et al.: Acetaminophen (paracetamol) improves pain and well-being in people with advanced cancer already receiving a strong opioid regimen: a randomized, double-blind, placebo-controlled cross-over trial. J Clin Oncol 22 (16): 3389-94, 2004. [PUBMED Abstract]
- Legeby M, Sandelin K, Wickman M, et al.: Analgesic efficacy of diclofenac in combination with morphine and paracetamol after mastectomy and immediate breast reconstruction. Acta Anaesthesiol Scand 49 (9): 1360-6, 2005. [PUBMED Abstract]
- Israel FJ, Parker G, Charles M, et al.: Lack of benefit from paracetamol (acetaminophen) for palliative cancer patients requiring high-dose strong opioids: a randomized, double-blind, placebo-controlled, crossover trial. J Pain Symptom Manage 39 (3): 548-54, 2010. [PUBMED Abstract]
- Tasmacioglu B, Aydinli I, Keskinbora K, et al.: Effect of intravenous administration of paracetamol on morphine consumption in cancer pain control. Support Care Cancer 17 (12): 1475-81, 2009. [PUBMED Abstract]
- Mitra R, Jones S: Adjuvant analgesics in cancer pain: a review. Am J Hosp Palliat Care 29 (1): 70-9, 2012. [PUBMED Abstract]
- Vardy J, Agar M: Nonopioid drugs in the treatment of cancer pain. J Clin Oncol 32 (16): 1677-90, 2014. [PUBMED Abstract]
- Nabal M, Librada S, Redondo MJ, et al.: The role of paracetamol and nonsteroidal anti-inflammatory drugs in addition to WHO Step III opioids in the control of pain in advanced cancer. A systematic review of the literature. Palliat Med 26 (4): 305-12, 2012. [PUBMED Abstract]
- Lexicomp Online. Hudson, Ohio: Lexi-Comp, Inc., 2021. Available online with subscription. Last accessed Feb. 9, 2024.
- Wiffen PJ, Wee B, Moore RA: Oral morphine for cancer pain. Cochrane Database Syst Rev 7: CD003868, 2013. [PUBMED Abstract]
- Bandieri E, Romero M, Ripamonti CI, et al.: Randomized Trial of Low-Dose Morphine Versus Weak Opioids in Moderate Cancer Pain. J Clin Oncol 34 (5): 436-42, 2016. [PUBMED Abstract]
- Schmidt-Hansen M, Bennett MI, Arnold S, et al.: Oxycodone for cancer-related pain. Cochrane Database Syst Rev 6: CD003870, 2022. [PUBMED Abstract]
- Bruera E, Belzile M, Pituskin E, et al.: Randomized, double-blind, cross-over trial comparing safety and efficacy of oral controlled-release oxycodone with controlled-release morphine in patients with cancer pain. J Clin Oncol 16 (10): 3222-9, 1998. [PUBMED Abstract]
- Bruera E, Sloan P, Mount B, et al.: A randomized, double-blind, double-dummy, crossover trial comparing the safety and efficacy of oral sustained-release hydromorphone with immediate-release hydromorphone in patients with cancer pain. Canadian Palliative Care Clinical Trials Group. J Clin Oncol 14 (5): 1713-7, 1996. [PUBMED Abstract]
- Stapleton SJ, Dyal BW, Boyd AD, et al.: Adherence to Analgesics Among Outpatients Seriously Ill With Cancer. Cancer Nurs 45 (5): 337-344, 2022 Sep-Oct 01. [PUBMED Abstract]
- Corli O, Montanari M, Deandrea S, et al.: An exploratory analysis on the effectiveness of four strong opioids in patients with cancer pain. Pain Med 13 (7): 897-907, 2012. [PUBMED Abstract]
- Naing C, Aung K, Racloz V, et al.: Safety and efficacy of transdermal buprenorphine for the relief of cancer pain. J Cancer Res Clin Oncol 139 (12): 1963-70, 2013. [PUBMED Abstract]
- Mesgarpour B, Griebler U, Glechner A, et al.: Extended-release opioids in the management of cancer pain: a systematic review of efficacy and safety. Eur J Pain 18 (5): 605-16, 2014. [PUBMED Abstract]
- Koivu L, Pölönen T, Stormi T, et al.: End-of-life pain medication among cancer patients in hospice settings. Anticancer Res 34 (11): 6581-4, 2014. [PUBMED Abstract]
- Reddy A, Tayjasanant S, Haider A, et al.: The opioid rotation ratio of strong opioids to transdermal fentanyl in cancer patients. Cancer 122 (1): 149-56, 2016. [PUBMED Abstract]
- Heiskanen T, Mätzke S, Haakana S, et al.: Transdermal fentanyl in cachectic cancer patients. Pain 144 (1-2): 218-22, 2009. [PUBMED Abstract]
- Reddy A, Yennurajalingam S, Desai H, et al.: The opioid rotation ratio of hydrocodone to strong opioids in cancer patients. Oncologist 19 (11): 1186-93, 2014. [PUBMED Abstract]
- Busse JW, Craigie S, Juurlink DN, et al.: Guideline for opioid therapy and chronic noncancer pain. CMAJ 189 (18): E659-E666, 2017. [PUBMED Abstract]
- Ripamonti C, Groff L, Brunelli C, et al.: Switching from morphine to oral methadone in treating cancer pain: what is the equianalgesic dose ratio? J Clin Oncol 16 (10): 3216-21, 1998. [PUBMED Abstract]
- Walker PW, Palla S, Pei BL, et al.: Switching from methadone to a different opioid: what is the equianalgesic dose ratio? J Palliat Med 11 (8): 1103-8, 2008. [PUBMED Abstract]
- Kress HG, Koch ED, Kosturski H, et al.: Tapentadol prolonged release for managing moderate to severe, chronic malignant tumor-related pain. Pain Physician 17 (4): 329-43, 2014 Jul-Aug. [PUBMED Abstract]
- Wiffen PJ, Derry S, Naessens K, et al.: Oral tapentadol for cancer pain. Cochrane Database Syst Rev (9): CD011460, 2015. [PUBMED Abstract]
- Escobar Y, Mañas A, Juliá J, et al.: Optimal management of breakthrough cancer pain (BCP). Clin Transl Oncol 15 (7): 526-34, 2013. [PUBMED Abstract]
- Oosten AW, Abrantes JA, Jönsson S, et al.: Treatment with subcutaneous and transdermal fentanyl: results from a population pharmacokinetic study in cancer patients. Eur J Clin Pharmacol 72 (4): 459-67, 2016. [PUBMED Abstract]
- Simon SM, Schwartzberg LS: A review of rapid-onset opioids for breakthrough pain in patients with cancer. J Opioid Manag 10 (3): 207-15, 2014 May-Jun. [PUBMED Abstract]
- McPherson ML, Walker KA, Davis MP, et al.: Safe and Appropriate Use of Methadone in Hospice and Palliative Care: Expert Consensus White Paper. J Pain Symptom Manage 57 (3): 635-645.e4, 2019. [PUBMED Abstract]
- Smith HS: Opioid metabolism. Mayo Clin Proc 84 (7): 613-24, 2009. [PUBMED Abstract]
- Chou R, Cruciani RA, Fiellin DA, et al.: Methadone safety: a clinical practice guideline from the American Pain Society and College on Problems of Drug Dependence, in collaboration with the Heart Rhythm Society. J Pain 15 (4): 321-37, 2014. [PUBMED Abstract]
- McLean S, Twomey F: Methods of Rotation From Another Strong Opioid to Methadone for the Management of Cancer Pain: A Systematic Review of the Available Evidence. J Pain Symptom Manage 50 (2): 248-59.e1, 2015. [PUBMED Abstract]
- Moksnes K, Dale O, Rosland JH, et al.: How to switch from morphine or oxycodone to methadone in cancer patients? a randomised clinical phase II trial. Eur J Cancer 47 (16): 2463-70, 2011. [PUBMED Abstract]
- Modesto-Lowe V, Brooks D, Petry N: Methadone deaths: risk factors in pain and addicted populations. J Gen Intern Med 25 (4): 305-9, 2010. [PUBMED Abstract]
- Cherny N, Ripamonti C, Pereira J, et al.: Strategies to manage the adverse effects of oral morphine: an evidence-based report. J Clin Oncol 19 (9): 2542-54, 2001. [PUBMED Abstract]
- McNicol E, Horowicz-Mehler N, Fisk RA, et al.: Management of opioid side effects in cancer-related and chronic noncancer pain: a systematic review. J Pain 4 (5): 231-56, 2003. [PUBMED Abstract]
- Smith HS, Smith JM, Seidner P: Opioid-induced nausea and vomiting. Ann Palliat Med 1 (2): 121-9, 2012. [PUBMED Abstract]
- Dorn S, Lembo A, Cremonini F: Opioid-induced bowel dysfunction: epidemiology, pathophysiology, diagnosis, and initial therapeutic approach. Am J Gastroenterol Suppl 2 (1): 31-7, 2014. [PUBMED Abstract]
- Bannister K: Opioid-induced hyperalgesia: where are we now? Curr Opin Support Palliat Care 9 (2): 116-21, 2015. [PUBMED Abstract]
- Ballantyne JC, Mao J: Opioid therapy for chronic pain. N Engl J Med 349 (20): 1943-53, 2003. [PUBMED Abstract]
- Benyamin R, Trescot AM, Datta S, et al.: Opioid complications and side effects. Pain Physician 11 (2 Suppl): S105-20, 2008. [PUBMED Abstract]
- Vella-Brincat J, Macleod AD: Adverse effects of opioids on the central nervous systems of palliative care patients. J Pain Palliat Care Pharmacother 21 (1): 15-25, 2007. [PUBMED Abstract]
- Slatkin N, Rhiner M: Treatment of opioid-induced delirium with acetylcholinesterase inhibitors: a case report. J Pain Symptom Manage 27 (3): 268-73, 2004. [PUBMED Abstract]
- Lim KH, Nguyen NN, Qian Y, et al.: Frequency, Outcomes, and Associated Factors for Opioid-Induced Neurotoxicity in Patients with Advanced Cancer Receiving Opioids in Inpatient Palliative Care. J Palliat Med 21 (12): 1698-1704, 2018. [PUBMED Abstract]
- Bruera E, Fainsinger R, MacEachern T, et al.: The use of methylphenidate in patients with incident cancer pain receiving regular opiates. A preliminary report. Pain 50 (1): 75-7, 1992. [PUBMED Abstract]
- Wilwerding MB, Loprinzi CL, Mailliard JA, et al.: A randomized, crossover evaluation of methylphenidate in cancer patients receiving strong narcotics. Support Care Cancer 3 (2): 135-8, 1995. [PUBMED Abstract]
- Ersek M, Cherrier MM, Overman SS, et al.: The cognitive effects of opioids. Pain Manag Nurs 5 (2): 75-93, 2004. [PUBMED Abstract]
- Lawlor PG: The panorama of opioid-related cognitive dysfunction in patients with cancer: a critical literature appraisal. Cancer 94 (6): 1836-53, 2002. [PUBMED Abstract]
- Morita T, Tei Y, Tsunoda J, et al.: Underlying pathologies and their associations with clinical features in terminal delirium of cancer patients. J Pain Symptom Manage 22 (6): 997-1006, 2001. [PUBMED Abstract]
- Ferrini F, Trang T, Mattioli TA, et al.: Morphine hyperalgesia gated through microglia-mediated disruption of neuronal Cl⁻ homeostasis. Nat Neurosci 16 (2): 183-92, 2013. [PUBMED Abstract]
- Simonnet G, Rivat C: Opioid-induced hyperalgesia: abnormal or normal pain? Neuroreport 14 (1): 1-7, 2003. [PUBMED Abstract]
- King T, Ossipov MH, Vanderah TW, et al.: Is paradoxical pain induced by sustained opioid exposure an underlying mechanism of opioid antinociceptive tolerance? Neurosignals 14 (4): 194-205, 2005. [PUBMED Abstract]
- Richebe P, Cahana A, Rivat C: Tolerance and opioid-induced hyperalgesia. Is a divorce imminent? Pain 153 (8): 1547-8, 2012. [PUBMED Abstract]
- Dahan A: Respiratory depression with opioids. J Pain Palliat Care Pharmacother 21 (1): 63-6, 2007. [PUBMED Abstract]
- Dahan A, Aarts L, Smith TW: Incidence, Reversal, and Prevention of Opioid-induced Respiratory Depression. Anesthesiology 112 (1): 226-38, 2010. [PUBMED Abstract]
- Clemens KE, Quednau I, Klaschik E: Is there a higher risk of respiratory depression in opioid-naïve palliative care patients during symptomatic therapy of dyspnea with strong opioids? J Palliat Med 11 (2): 204-16, 2008. [PUBMED Abstract]
- Clemens KE, Klaschik E: Symptomatic therapy of dyspnea with strong opioids and its effect on ventilation in palliative care patients. J Pain Symptom Manage 33 (4): 473-81, 2007. [PUBMED Abstract]
- Clemens KE, Quednau I, Klaschik E: Use of oxygen and opioids in the palliation of dyspnoea in hypoxic and non-hypoxic palliative care patients: a prospective study. Support Care Cancer 17 (4): 367-77, 2009. [PUBMED Abstract]
- Clemens KE, Klaschik E: Dyspnoea associated with anxiety–symptomatic therapy with opioids in combination with lorazepam and its effect on ventilation in palliative care patients. Support Care Cancer 19 (12): 2027-33, 2011. [PUBMED Abstract]
- Moulin DE, Iezzi A, Amireh R, et al.: Randomised trial of oral morphine for chronic non-cancer pain. Lancet 347 (8995): 143-7, 1996. [PUBMED Abstract]
- Mannix KA: Palliation of nausea and vomiting. In: Doyle D, Hanks GW, MacDonald N, eds.: Oxford Textbook of Palliative Medicine. Oxford University Press, 1998, pp 489-499.
- Swegle JM, Logemann C: Management of common opioid-induced adverse effects. Am Fam Physician 74 (8): 1347-54, 2006. [PUBMED Abstract]
- Derby S, Portenoy RK: Assessment and management of opioid-induced constipation. In: Portenoy RK, Bruera E, eds.: Topics in Palliative Care. Volume 1. Oxford University Press, 1997, pp 95-112.
- Hawley PH, Byeon JJ: A comparison of sennosides-based bowel protocols with and without docusate in hospitalized patients with cancer. J Palliat Med 11 (4): 575-81, 2008. [PUBMED Abstract]
- Tarumi Y, Wilson MP, Szafran O, et al.: Randomized, double-blind, placebo-controlled trial of oral docusate in the management of constipation in hospice patients. J Pain Symptom Manage 45 (1): 2-13, 2013. [PUBMED Abstract]
- Thomas J, Karver S, Cooney GA, et al.: Methylnaltrexone for opioid-induced constipation in advanced illness. N Engl J Med 358 (22): 2332-43, 2008. [PUBMED Abstract]
- Chey WD, Webster L, Sostek M, et al.: Naloxegol for opioid-induced constipation in patients with noncancer pain. N Engl J Med 370 (25): 2387-96, 2014. [PUBMED Abstract]
- Troxyca ER (Oxycodone Hydrochloride and Naltrexone Hydrochloride) Extended-Release Capsules, for Oral Use. New York, NY: Pfizer Inc., 2016. Available online. Last accessed Feb. 9, 2024.
- Vuong C, Van Uum SH, O’Dell LE, et al.: The effects of opioids and opioid analogs on animal and human endocrine systems. Endocr Rev 31 (1): 98-132, 2010. [PUBMED Abstract]
- Daniell HW, Lentz R, Mazer NA: Open-label pilot study of testosterone patch therapy in men with opioid-induced androgen deficiency. J Pain 7 (3): 200-10, 2006. [PUBMED Abstract]
- Makman MH: Morphine receptors in immunocytes and neurons. Adv Neuroimmunol 4 (2): 69-82, 1994. [PUBMED Abstract]
- Haberer JP, Schoeffler P, Couderc E, et al.: Fentanyl pharmacokinetics in anaesthetized patients with cirrhosis. Br J Anaesth 54 (12): 1267-70, 1982. [PUBMED Abstract]
- Novick DM, Kreek MJ, Fanizza AM, et al.: Methadone disposition in patients with chronic liver disease. Clin Pharmacol Ther 30 (3): 353-62, 1981. [PUBMED Abstract]
- Hasselström J, Eriksson S, Persson A, et al.: The metabolism and bioavailability of morphine in patients with severe liver cirrhosis. Br J Clin Pharmacol 29 (3): 289-97, 1990. [PUBMED Abstract]
- OxyContin (Oxycodone Hydrochloride Extended-Release Tablets), for Oral Use. Stamford, Conn.: Purdue Pharma L.P., 2021. Available online. Last accessed Feb. 9, 2024.
- Opana ER (Oxymorphone Hydrochloride) Extended-Release Tablets, for Oral Use. Malvern, Pa: Endo Pharmaceuticals Inc., 2019. Available online. Last accessed September 7, 2023.
- Dean M: Opioids in renal failure and dialysis patients. J Pain Symptom Manage 28 (5): 497-504, 2004. [PUBMED Abstract]
- Paramanandam G, Prommer E, Schwenke DC: Adverse effects in hospice patients with chronic kidney disease receiving hydromorphone. J Palliat Med 14 (9): 1029-33, 2011. [PUBMED Abstract]
- Lee MA, Leng ME, Tiernan EJ: Retrospective study of the use of hydromorphone in palliative care patients with normal and abnormal urea and creatinine. Palliat Med 15 (1): 26-34, 2001. [PUBMED Abstract]
- Fine PG, Portenoy RK; Ad Hoc Expert Panel on Evidence Review and Guidelines for Opioid Rotation: Establishing “best practices” for opioid rotation: conclusions of an expert panel. J Pain Symptom Manage 38 (3): 418-25, 2009. [PUBMED Abstract]
- Smith HS, Peppin JF: Toward a systematic approach to opioid rotation. J Pain Res 7: 589-608, 2014. [PUBMED Abstract]
- Reddy A, Yennurajalingam S, Pulivarthi K, et al.: Frequency, outcome, and predictors of success within 6 weeks of an opioid rotation among outpatients with cancer receiving strong opioids. Oncologist 18 (2): 212-20, 2013. [PUBMED Abstract]
- Hui D, Shamieh O, Paiva CE, et al.: Minimal clinically important differences in the Edmonton Symptom Assessment Scale in cancer patients: A prospective, multicenter study. Cancer 121 (17): 3027-35, 2015. [PUBMED Abstract]
- Potter VT, Wiseman CE, Dunn SM, et al.: Patient barriers to optimal cancer pain control. Psychooncology 12 (2): 153-60, 2003. [PUBMED Abstract]
- Ward SE, Goldberg N, Miller-McCauley V, et al.: Patient-related barriers to management of cancer pain. Pain 52 (3): 319-24, 1993. [PUBMED Abstract]
- Jacobsen R, Sjøgren P, Møldrup C, et al.: Physician-related barriers to cancer pain management with opioid analgesics: a systematic review. J Opioid Manag 3 (4): 207-14, 2007 Jul-Aug. [PUBMED Abstract]
- Dowell D, Haegerich TM, Chou R: CDC Guideline for Prescribing Opioids for Chronic Pain–United States, 2016. JAMA 315 (15): 1624-45, 2016. [PUBMED Abstract]
- Jairam V, Yang DX, Pasha S, et al.: Temporal Trends in Opioid Prescribing Patterns Among Oncologists in the Medicare Population. J Natl Cancer Inst 113 (3): 274-281, 2021. [PUBMED Abstract]
- Chen Y, Spillane S, Shiels MS, et al.: Trends in Opioid Use Among Cancer Patients in the United States: 2013-2018. JNCI Cancer Spectr 6 (1): , 2022. [PUBMED Abstract]
- Enzinger AC, Ghosh K, Keating NL, et al.: US Trends in Opioid Access Among Patients With Poor Prognosis Cancer Near the End-of-Life. J Clin Oncol 39 (26): 2948-2958, 2021. [PUBMED Abstract]
- Hu X, Brock KE, Effinger KE, et al.: Changes in Opioid Prescriptions and Potential Misuse and Substance Use Disorders Among Childhood Cancer Survivors Following the 2016 Opioid Prescribing Guideline. JAMA Oncol 8 (11): 1658-1662, 2022. [PUBMED Abstract]
- Enzinger AC, Ghosh K, Keating NL, et al.: Racial and Ethnic Disparities in Opioid Access and Urine Drug Screening Among Older Patients With Poor-Prognosis Cancer Near the End of Life. J Clin Oncol 41 (14): 2511-2522, 2023. [PUBMED Abstract]
- Canick JE, Bhardwaj A, Patel A, et al.: Sociodemographic Differences in Patient-Reported Pain and Pain Management of Patients With Head and Neck Cancer in a Community Oncology Setting. JCO Oncol Pract 19 (3): e397-e406, 2023. [PUBMED Abstract]
- Centers for Disease Control and Prevention: The Drug Overdose Epidemic: Behind the Numbers. Atlanta, Ga: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, 2023. Available online. Last accessed Feb. 9, 2024.
- Højsted J, Sjøgren P: Addiction to opioids in chronic pain patients: a literature review. Eur J Pain 11 (5): 490-518, 2007. [PUBMED Abstract]
- Koyyalagunta D, Burton AW, Toro MP, et al.: Opioid abuse in cancer pain: report of two cases and presentation of an algorithm of multidisciplinary care. Pain Physician 14 (4): E361-71, 2011 Jul-Aug. [PUBMED Abstract]
- Roberts AW, Eiffert S, Wulff-Burchfield EM, et al.: Opioid Use Disorder and Overdose in Older Adults With Breast, Colorectal, or Prostate Cancer. J Natl Cancer Inst 113 (4): 425-433, 2021. [PUBMED Abstract]
- Paice JA, Von Roenn JH: Under- or overtreatment of pain in the patient with cancer: how to achieve proper balance. J Clin Oncol 32 (16): 1721-6, 2014. [PUBMED Abstract]
- Lee JS, Hu HM, Edelman AL, et al.: New Persistent Opioid Use Among Patients With Cancer After Curative-Intent Surgery. J Clin Oncol 35 (36): 4042-4049, 2017. [PUBMED Abstract]
- Passik SD: Issues in long-term opioid therapy: unmet needs, risks, and solutions. Mayo Clin Proc 84 (7): 593-601, 2009. [PUBMED Abstract]
- Passik SD, Kirsh KL: The need to identify predictors of aberrant drug-related behavior and addiction in patients being treated with opioids for pain. Pain Med 4 (2): 186-9, 2003. [PUBMED Abstract]
- Kwon JH, Hui D, Bruera E: A Pilot Study To Define Chemical Coping in Cancer Patients Using the Delphi Method. J Palliat Med 18 (8): 703-6, 2015. [PUBMED Abstract]
- Gourlay DL, Heit HA: Pain and addiction: managing risk through comprehensive care. J Addict Dis 27 (3): 23-30, 2008. [PUBMED Abstract]
- Webster LR, Webster RM: Predicting aberrant behaviors in opioid-treated patients: preliminary validation of the Opioid Risk Tool. Pain Med 6 (6): 432-42, 2005 Nov-Dec. [PUBMED Abstract]
- Butler SF, Fernandez K, Benoit C, et al.: Validation of the revised Screener and Opioid Assessment for Patients with Pain (SOAPP-R). J Pain 9 (4): 360-72, 2008. [PUBMED Abstract]
- Coambs RB, Jarry JL, Santhiapillai AC, et al.: The SISAP: a new screening instrument for identifying potential opioid abusers in the management of chronic nonmalignant pain within general medical practice. Pain Res Manag 1 (3): 155-62, 1996.
- Paice JA, Portenoy R, Lacchetti C, et al.: Management of Chronic Pain in Survivors of Adult Cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol 34 (27): 3325-45, 2016. [PUBMED Abstract]
- The use of opioids for the treatment of chronic pain. A consensus statement from the American Academy of Pain Medicine and the American Pain Society. Clin J Pain 13 (1): 6-8, 1997. [PUBMED Abstract]
- Wiedemer NL, Harden PS, Arndt IO, et al.: The opioid renewal clinic: a primary care, managed approach to opioid therapy in chronic pain patients at risk for substance abuse. Pain Med 8 (7): 573-84, 2007 Oct-Nov. [PUBMED Abstract]
- Gourlay DL, Heit HA, Almahrezi A: Universal precautions in pain medicine: a rational approach to the treatment of chronic pain. Pain Med 6 (2): 107-12, 2005 Mar-Apr. [PUBMED Abstract]
- Arthur JA: Urine Drug Testing in Cancer Pain Management. Oncologist 25 (2): 99-104, 2020. [PUBMED Abstract]
- Chindalore VL, Craven RA, Yu KP, et al.: Adding ultralow-dose naltrexone to oxycodone enhances and prolongs analgesia: a randomized, controlled trial of Oxytrex. J Pain 6 (6): 392-9, 2005. [PUBMED Abstract]
- Setnik B, Roland CL, Cleveland JM, et al.: The abuse potential of Remoxy(®), an extended-release formulation of oxycodone, compared with immediate- and extended-release oxycodone. Pain Med 12 (4): 618-31, 2011. [PUBMED Abstract]
- Dworkin RH, O’Connor AB, Audette J, et al.: Recommendations for the pharmacological management of neuropathic pain: an overview and literature update. Mayo Clin Proc 85 (3 Suppl): S3-14, 2010. [PUBMED Abstract]
- Pachman DR, Watson JC, Loprinzi CL: Therapeutic strategies for cancer treatment related peripheral neuropathies. Curr Treat Options Oncol 15 (4): 567-80, 2014. [PUBMED Abstract]
- Pachman DR, Barton DL, Watson JC, et al.: Chemotherapy-induced peripheral neuropathy: prevention and treatment. Clin Pharmacol Ther 90 (3): 377-87, 2011. [PUBMED Abstract]
- Paulsen Ø, Aass N, Kaasa S, et al.: Do corticosteroids provide analgesic effects in cancer patients? A systematic literature review. J Pain Symptom Manage 46 (1): 96-105, 2013. [PUBMED Abstract]
- Paulsen O, Klepstad P, Rosland JH, et al.: Efficacy of methylprednisolone on pain, fatigue, and appetite loss in patients with advanced cancer using opioids: a randomized, placebo-controlled, double-blind trial. J Clin Oncol 32 (29): 3221-8, 2014. [PUBMED Abstract]
- Leppert W, Buss T: The role of corticosteroids in the treatment of pain in cancer patients. Curr Pain Headache Rep 16 (4): 307-13, 2012. [PUBMED Abstract]
- Portenoy RK, Frager G: Pain management: pharmacological approaches. In: von Gunten CF, ed.: Palliative Care and Rehabilitation of Cancer Patients. Kluwer Academic Publishers, 1999, pp 1-29.
- Watanabe S, Bruera E: Corticosteroids as adjuvant analgesics. J Pain Symptom Manage 9 (7): 442-5, 1994. [PUBMED Abstract]
- Chow E, Meyer RM, Ding K, et al.: Dexamethasone in the prophylaxis of radiation-induced pain flare after palliative radiotherapy for bone metastases: a double-blind, randomised placebo-controlled, phase 3 trial. Lancet Oncol 16 (15): 1463-72, 2015. [PUBMED Abstract]
- Rosen LS, Gordon D, Antonio BS, et al.: Zoledronic acid versus pamidronate in the treatment of skeletal metastases in patients with breast cancer or osteolytic lesions of multiple myeloma: a phase III, double-blind, comparative trial. Cancer J 7 (5): 377-87, 2001 Sep-Oct. [PUBMED Abstract]
- Wardley A, Davidson N, Barrett-Lee P, et al.: Zoledronic acid significantly improves pain scores and quality of life in breast cancer patients with bone metastases: a randomised, crossover study of community vs hospital bisphosphonate administration. Br J Cancer 92 (10): 1869-76, 2005. [PUBMED Abstract]
- Rosen LS, Gordon D, Tchekmedyian S, et al.: Zoledronic acid versus placebo in the treatment of skeletal metastases in patients with lung cancer and other solid tumors: a phase III, double-blind, randomized trial–the Zoledronic Acid Lung Cancer and Other Solid Tumors Study Group. J Clin Oncol 21 (16): 3150-7, 2003. [PUBMED Abstract]
- Weinfurt KP, Anstrom KJ, Castel LD, et al.: Effect of zoledronic acid on pain associated with bone metastasis in patients with prostate cancer. Ann Oncol 17 (6): 986-9, 2006. [PUBMED Abstract]
- Van Poznak CH, Temin S, Yee GC, et al.: American Society of Clinical Oncology executive summary of the clinical practice guideline update on the role of bone-modifying agents in metastatic breast cancer. J Clin Oncol 29 (9): 1221-7, 2011. [PUBMED Abstract]
- Kyle RA, Yee GC, Somerfield MR, et al.: American Society of Clinical Oncology 2007 clinical practice guideline update on the role of bisphosphonates in multiple myeloma. J Clin Oncol 25 (17): 2464-72, 2007. [PUBMED Abstract]
- Qi WX, Tang LN, He AN, et al.: Risk of osteonecrosis of the jaw in cancer patients receiving denosumab: a meta-analysis of seven randomized controlled trials. Int J Clin Oncol 19 (2): 403-10, 2014. [PUBMED Abstract]
- Henry DH, Costa L, Goldwasser F, et al.: Randomized, double-blind study of denosumab versus zoledronic acid in the treatment of bone metastases in patients with advanced cancer (excluding breast and prostate cancer) or multiple myeloma. J Clin Oncol 29 (9): 1125-32, 2011. [PUBMED Abstract]
- Sivolella S, Lumachi F, Stellini E, et al.: Denosumab and anti-angiogenetic drug-related osteonecrosis of the jaw: an uncommon but potentially severe disease. Anticancer Res 33 (5): 1793-7, 2013. [PUBMED Abstract]
- Hoskin P, Sundar S, Reczko K, et al.: A Multicenter Randomized Trial of Ibandronate Compared With Single-Dose Radiotherapy for Localized Metastatic Bone Pain in Prostate Cancer. J Natl Cancer Inst 107 (10): , 2015. [PUBMED Abstract]
- Peddi P, Lopez-Olivo MA, Pratt GF, et al.: Denosumab in patients with cancer and skeletal metastases: a systematic review and meta-analysis. Cancer Treat Rev 39 (1): 97-104, 2013. [PUBMED Abstract]
- Shapiro CL, Moriarty JP, Dusetzina S, et al.: Cost-Effectiveness Analysis of Monthly Zoledronic Acid, Zoledronic Acid Every 3 Months, and Monthly Denosumab in Women With Breast Cancer and Skeletal Metastases: CALGB 70604 (Alliance). J Clin Oncol 35 (35): 3949-3955, 2017. [PUBMED Abstract]
- Bell RF, Eccleston C, Kalso EA: Ketamine as an adjuvant to opioids for cancer pain. Cochrane Database Syst Rev 11: CD003351, 2012. [PUBMED Abstract]
- Hardy J, Quinn S, Fazekas B, et al.: Randomized, double-blind, placebo-controlled study to assess the efficacy and toxicity of subcutaneous ketamine in the management of cancer pain. J Clin Oncol 30 (29): 3611-7, 2012. [PUBMED Abstract]
Modalities for Pain Control: Other Approaches
Pain Procedures
While pharmacological therapy using the World Health Organization (WHO) guidelines effectively manages most cancer pain, approximately 10% to 20% of patients will have refractory pain or excessive side effects.[1] For patients with refractory pain or specific regional pain syndromes, an interventional approach to treating pain has been proposed as the fourth step on the WHO pain relief ladder. Some common interventions and their evidence of benefit are discussed below.
Nerve blocks
The celiac plexus block, used primarily for patients with upper abdominal pain from pancreatic cancer, is the most commonly employed neurolytic blockade of the sympathetic axis, followed by the superior hypogastric plexus block and the ganglion of impar block for patients with lower abdominal or pelvic pain. Traditionally, the autonomic neural blockade was reserved for patients with inadequate response to oral opioids, but some researchers have suggested that the intervention—which is associated with decreased pain, reduced opioid consumption, improved performance status, and few complications—is considered a first-line approach.[2,3]
For patients with regional pain, a peripheral nerve block infusing a local anesthetic can achieve local pain control. This approach can be applied to any peripheral nerve, including the femoral, sciatic, paravertebral, brachial plexus, and interpleural nerves.[4]
Neuroaxial delivery of analgesia
When patients have pain that persists despite high doses of opioids and other analgesics or have intolerable side effects to oral opioids—such as delirium, sedation, or nausea—an alternative route of delivery may be considered. Compared with intravenous administration of opioids, epidural and intrathecal routes of delivery are 10 and 100 times more potent, respectively. Such routes of delivery allow high doses of analgesics to be administered with less systemic absorption and fewer side effects.[5]
One study that randomly assigned patients to receive either an implantable drug delivery system or comprehensive medical management found that patients receiving the analgesic through the implantable pump had less pain, less toxicity, and longer survival at 6 months.[6] While the survival benefit did not persist in other studies, the intrathecal pump may be an option for selected patients with refractory pain and a life expectancy longer than 3 months.[7] However, intrathecal pumps may make it difficult for patients to access hospice care because of care needs and cost issues, and they cannot effectively treat pain that is predominantly related to psychological distress.[8] For patients with shorter life expectancies, placement of an epidural catheter may be a safe and effective technique.[4]
Cordotomy
Cordotomy is reserved for pain refractory to other approaches and is done less commonly today. It is most effective in treating unilateral somatic pain from the torso to the lower extremities. The available literature suggests a high rate of efficacy, with 60% to 80% complete pain relief immediately after the procedure, falling to 50% at 12 months. Cordotomy is generally reserved for patients considered to be in the last 2 years of life, with pain refractory to other approaches, and may be done via the open route or the percutaneous route.[9–11]
For patients with either regional pain syndromes or pain refractory to escalating systemic medications, the cancer clinician may consult with a pain specialist or neurosurgeon to consider an interventional approach to pain control.
Palliative Care Referral
Palliative care, which is specialized medical care for people with serious illnesses with the goal to maximize quality of life (QOL) for both patients and families, can provide expert assessment and management of pain and other nonpain symptoms. Palliative care providers work in interdisciplinary teams that include the following:
- Physicians.
- Nurses.
- Mental health specialists.
- Social workers.
- Chaplains.
- Pharmacists.
- Dieticians.
For patients with refractory pain, prominent nonpain symptoms, or intense psychosocial distress, a referral to palliative care may be appropriate, where available. Many palliative care teams now call themselves supportive care teams because this term is more acceptable to many referring providers and to some patients and families.[12,13]
Palliative care specialists may also help manage patients with multiple comorbidities, those requiring higher doses of opioids, and those with a history of substance use disorder or complex psychosocial dynamics that can complicate the management of pain and adherence to recommended medications. Most palliative care specialists have experience using methadone for pain.
The role of specialty palliative care integrated into cancer care has been well studied, with studies showing that early integration of specialty palliative care into cancer care reduces symptom burden and enhances QOL for both patients and families [14–17] and may prolong life.[14] For more information, see Planning the Transition to End-of-Life Care in Advanced Cancer.
External-Beam Radiation Therapy
Palliative radiation therapy represents an effective modality for pain related to advanced cancer. Pain related to bone metastases, skin lesions, or isolated tumor lesions may be relieved by a short course of radiation therapy. Patient selection can be important regarding the likelihood of benefit from radiation therapy.[18] In one study, patients with hematologic tumors, a neuropathic component of the index pain, and no previous treatment with opioid analgesics before radiation therapy were more likely to experience pain palliation after radiation therapy.[19]
For bone metastases, radiation is often delivered as 8 Gy in a single fraction, 20 Gy in five fractions, 24 Gy in six fractions, or 30 Gy in ten fractions. A Cochrane review that included 11 randomized trials consisting of 3,435 patients showed that single-fraction radiation therapy for bone pain provided a similar overall response rate (60% vs. 59%) and complete response rate (34% vs. 32%), compared with multifraction radiation therapy.[20] However, patients who received single-fraction radiation therapy had a higher rate of re-treatment (22% vs. 7%) and a higher rate of pathological fracture (3% vs. 1.6%).[20] This finding was consistent with other systematic reviews.[21] In the Dutch Bone Metastasis Study, the average time to first pain relief was 3 weeks; the peak effect was achieved in 4 to 6 weeks; and the mean duration of response was approximately 30 weeks.[22,23] Single-fraction radiation has several potential advantages:
- Greater convenience.
- Lower cost.
- Less breakthrough pain associated with transportation to the radiation facility and with getting on and off the radiation table.
A study published in 2019 evaluated a higher-dosage (Gy) single-fraction stereotactic body radiation therapy (SBRT) versus multifraction radiation therapy (MFRT), in which patients with primarily nonspine bone metastases received either single-fraction SBRT (12 Gy for ≥4-cm lesions or 16 Gy for <4-cm lesions) or MFRT to 30 Gy in ten fractions. This randomized phase II trial demonstrated improved pain at 2 weeks, 3 months, and 9 months, without differences in treatment-related toxicity and with no increase with re-treatment rates that had been seen in previous single-fraction studies, done largely with 8 Gy. Patients who received the higher-dose SBRT had improved 1- and 2-year survival rates. The authors concluded that the higher dose of single-fraction SBRT is safe and suggested that this could become the standard of care, if confirmed in phase III studies.[24][Level of evidence: I]
Re-irradiation may be considered for selected patients who derive no or partial pain relief with first-time radiation therapy, or who develop worsening pain after an initial response. Re-irradiation typically occurs at least 4 weeks after the first radiation treatment. A systematic review that examined re-irradiation for bone metastases included 15 studies and reported a complete response rate of 20% and a partial response rate of 50%.[25] Re-irradiation was generally well tolerated.[25] In a secondary analysis of the National Cancer Institute of Canada (NCIC) Clinical Trials Group Symptom Control Trial SC.20, which examined outcomes of 847 patients who underwent palliative re-irradiation of painful bone metastases, the team found no differences in pain relief or side effects across age or gender demographics. Women and younger patients reported greater improvements in QOL.[26] Serious adverse effects such as spinal cord compression and pathological fracture were infrequent (<3%). A randomized controlled trial compared a single fraction (8 Gy) with multiple fractions (20 Gy over 5 days) of re-irradiation and found similar response rates at 2 months in an intention-to-treat analysis (28% vs. 32%; P = .02).[27]
A potential side effect of palliative radiation for painful bone metastases is a temporary increase in pain level, i.e., a pain flare. Pain flares occur in about 40% of patients and may be quite distressing. One study [28] randomly assigned 298 patients, who were scheduled to receive a single 8-Gy dose of radiation, to receive either placebo or dexamethasone 8 mg on days 0 to 4. Fewer patients in the dexamethasone group experienced pain flares (26% vs. 35%; P = .05). Potentially serious hyperglycemia was seen in only two patients in the dexamethasone group. The study supports the use of prophylactic dexamethasone in this setting.
In a secondary analysis of the NCIC Clinical Trials Group Symptom Control Trial SC.23, the authors investigated pain and QOL at days 10 and 42 after radiation therapy, with the aim of determining whether there are differences in QOL between responders and nonresponders.[29] Overall, 40% of patients experienced pain reduction and improvement in QOL at day 10, with continued improvement in QOL at day 42. Compared with baseline, patients responding to radiation experienced significantly increased improvements in the physical, emotional, and global domains of the day-42 QOL tool.
Radionuclides
Patients with multiple sites of symptomatic osteoblastic bone metastases may consider radionuclides such as strontium chloride Sr 89 or samarium Sm 153 (153Sm), which are beta-emitters. Two double-blind randomized trials support the superiority of 153Sm over placebo in providing pain control and reducing analgesic use.[30,31] The overall response varies between 30% and 80%, with onset of pain relief within the first week; some patients report a long-lasting benefit (up to 18 months). The most common toxicities are pain flare and cytopenias. Pain flare typically occurs in approximately 10% of patients within the first 24 to 48 hours of administration and may be treated with corticosteroids or opioids.[32] Leukopenia and thrombocytopenia are sometimes seen, with a nadir of 4 weeks posttreatment and recovery by 8 weeks. Contraindications to radionuclide therapy include a poor performance status (Karnofsky Performance Status score <50%) and a short life expectancy (<3 months).
Radium Ra 223-dichloride (223Ra-dichloride) (an alpha-emitter) is approved for use in patients with castration-resistant prostate cancer. A phase III randomized trial compared 223Ra-dichloride with placebo in a 2:1 ratio. Among the 921 symptomatic patients enrolled, those who received 223Ra-dichloride had a prolonged time to first symptomatic skeletal event (15.6 months vs. 9.8 months, P < .0001), in addition to prolonged overall survival (14.9 months vs. 11.3 months, P < .001).[33]
Physical Medicine and Rehabilitation
Patients with cancer and pain may experience loss of strength, mobility, and, ultimately, functional status secondary to the cause of pain, (e.g., vertebral metastases, incident pain, and chronic nonmalignant pain). Therefore, pain and functional status may improve with physical or occupational therapy, treatments for strengthening and stretching, and the use of assistive devices.[34] Referral to a physiatrist (a physician who specializes in rehabilitation medicine) who could create a comprehensive plan may benefit the patient. In addition, some physiatrists practice interventional pain medicine.
Integrative Therapy
Patients with cancer frequently use complementary or alternative medicines or interventions (CAM).[35] One of the stated benefits of CAM is pain relief. However, a meta-analysis of multi-institutional, randomized, controlled trials for cancer-related pain concluded that methodological flaws hampered interpretation of the few available studies. There were brief positive effects in favor of CAM for acupuncture, support groups, hypnosis, and herbal supplements.[36] For more information, see the summaries on Integrative, Alternative, and Complementary Therapies.
References
- McHugh ME, Miller-Saultz D, Wuhrman E, et al.: Interventional pain management in the palliative care patient. Int J Palliat Nurs 18 (9): 426-8, 430-3, 2012. [PUBMED Abstract]
- Tei Y, Morita T, Nakaho T, et al.: Treatment efficacy of neural blockade in specialized palliative care services in Japan: a multicenter audit survey. J Pain Symptom Manage 36 (5): 461-7, 2008. [PUBMED Abstract]
- Bhatnagar S, Khanna S, Roshni S, et al.: Early ultrasound-guided neurolysis for pain management in gastrointestinal and pelvic malignancies: an observational study in a tertiary care center of urban India. Pain Pract 12 (1): 23-32, 2012. [PUBMED Abstract]
- Chambers WA: Nerve blocks in palliative care. Br J Anaesth 101 (1): 95-100, 2008. [PUBMED Abstract]
- Smyth CE, Jarvis V, Poulin P: Brief review: Neuraxial analgesia in refractory malignant pain. Can J Anaesth 61 (2): 141-53, 2014. [PUBMED Abstract]
- Smith TJ, Staats PS, Deer T, et al.: Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol 20 (19): 4040-9, 2002. [PUBMED Abstract]
- Smith TJ, Coyne PJ: Implantable drug delivery systems (IDDS) after failure of comprehensive medical management (CMM) can palliate symptoms in the most refractory cancer pain patients. J Palliat Med 8 (4): 736-42, 2005. [PUBMED Abstract]
- Reddy A, Yennurajalingam S, de la Cruz M, et al.: Factors associated with survival after opioid rotation in cancer patients presenting to an outpatient supportive care center. J Pain Symptom Manage 48 (1): 92-8, 2014. [PUBMED Abstract]
- Siegfried J: Electrostimulation and neurosurgical measures in cancer pain. Recent Results Cancer Res 108: 28-32, 1988. [PUBMED Abstract]
- Lahuerta J, Bowsher D, Lipton S, et al.: Percutaneous cervical cordotomy: a review of 181 operations on 146 patients with a study on the location of “pain fibers” in the C-2 spinal cord segment of 29 cases. J Neurosurg 80 (6): 975-85, 1994. [PUBMED Abstract]
- Lahuerta J, Lipton S, Wells JC: Percutaneous cervical cordotomy: results and complications in a recent series of 100 patients. Ann R Coll Surg Engl 67 (1): 41-4, 1985. [PUBMED Abstract]
- Fadul N, Elsayem A, Palmer JL, et al.: Supportive versus palliative care: what’s in a name?: a survey of medical oncologists and midlevel providers at a comprehensive cancer center. Cancer 115 (9): 2013-21, 2009. [PUBMED Abstract]
- Dalal S, Palla S, Hui D, et al.: Association between a name change from palliative to supportive care and the timing of patient referrals at a comprehensive cancer center. Oncologist 16 (1): 105-11, 2011. [PUBMED Abstract]
- Temel JS, Greer JA, Muzikansky A, et al.: Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363 (8): 733-42, 2010. [PUBMED Abstract]
- Zimmermann C, Swami N, Krzyzanowska M, et al.: Early palliative care for patients with advanced cancer: a cluster-randomised controlled trial. Lancet 383 (9930): 1721-30, 2014. [PUBMED Abstract]
- Bakitas M, Lyons KD, Hegel MT, et al.: The project ENABLE II randomized controlled trial to improve palliative care for rural patients with advanced cancer: baseline findings, methodological challenges, and solutions. Palliat Support Care 7 (1): 75-86, 2009. [PUBMED Abstract]
- Bakitas MA, Tosteson TD, Li Z, et al.: Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. J Clin Oncol 33 (13): 1438-45, 2015. [PUBMED Abstract]
- Habberstad R, Frøseth TCS, Aass N, et al.: Clinical Predictors for Analgesic Response to Radiotherapy in Patients with Painful Bone Metastases. J Pain Symptom Manage 62 (4): 681-690, 2021. [PUBMED Abstract]
- Saito T, Toya R, Tomitaka E, et al.: Predictors of Pain Palliation After Radiation Therapy for Painful Tumors: A Prospective Observational Study. Int J Radiat Oncol Biol Phys 101 (5): 1061-1068, 2018. [PUBMED Abstract]
- Sze WM, Shelley M, Held I, et al.: Palliation of metastatic bone pain: single fraction versus multifraction radiotherapy – a systematic review of the randomised trials. Cochrane Database Syst Rev (2): CD004721, 2004. [PUBMED Abstract]
- Chow E, Zeng L, Salvo N, et al.: Update on the systematic review of palliative radiotherapy trials for bone metastases. Clin Oncol (R Coll Radiol) 24 (2): 112-24, 2012. [PUBMED Abstract]
- van der Linden YM, Lok JJ, Steenland E, et al.: Single fraction radiotherapy is efficacious: a further analysis of the Dutch Bone Metastasis Study controlling for the influence of retreatment. Int J Radiat Oncol Biol Phys 59 (2): 528-37, 2004. [PUBMED Abstract]
- van der Linden YM, Steenland E, van Houwelingen HC, et al.: Patients with a favourable prognosis are equally palliated with single and multiple fraction radiotherapy: results on survival in the Dutch Bone Metastasis Study. Radiother Oncol 78 (3): 245-53, 2006. [PUBMED Abstract]
- Nguyen QN, Chun SG, Chow E, et al.: Single-Fraction Stereotactic vs Conventional Multifraction Radiotherapy for Pain Relief in Patients With Predominantly Nonspine Bone Metastases: A Randomized Phase 2 Trial. JAMA Oncol 5 (6): 872-878, 2019. [PUBMED Abstract]
- Wong E, Hoskin P, Bedard G, et al.: Re-irradiation for painful bone metastases – a systematic review. Radiother Oncol 110 (1): 61-70, 2014. [PUBMED Abstract]
- Chow R, Ding K, Ganesh V, et al.: Gender and age make no difference in the re-irradiation of painful bone metastases: A secondary analysis of the NCIC CTG SC.20 randomized trial. Radiother Oncol 126 (3): 541-546, 2018. [PUBMED Abstract]
- Chow E, van der Linden YM, Roos D, et al.: Single versus multiple fractions of repeat radiation for painful bone metastases: a randomised, controlled, non-inferiority trial. Lancet Oncol 15 (2): 164-71, 2014. [PUBMED Abstract]
- Chow E, Meyer RM, Ding K, et al.: Dexamethasone in the prophylaxis of radiation-induced pain flare after palliative radiotherapy for bone metastases: a double-blind, randomised placebo-controlled, phase 3 trial. Lancet Oncol 16 (15): 1463-72, 2015. [PUBMED Abstract]
- McDonald R, Ding K, Brundage M, et al.: Effect of Radiotherapy on Painful Bone Metastases: A Secondary Analysis of the NCIC Clinical Trials Group Symptom Control Trial SC.23. JAMA Oncol 3 (7): 953-959, 2017. [PUBMED Abstract]
- Serafini AN, Houston SJ, Resche I, et al.: Palliation of pain associated with metastatic bone cancer using samarium-153 lexidronam: a double-blind placebo-controlled clinical trial. J Clin Oncol 16 (4): 1574-81, 1998. [PUBMED Abstract]
- Sartor O, Reid RH, Bushnell DL, et al.: Safety and efficacy of repeat administration of samarium Sm-153 lexidronam to patients with metastatic bone pain. Cancer 109 (3): 637-43, 2007. [PUBMED Abstract]
- Resche I, Chatal JF, Pecking A, et al.: A dose-controlled study of 153Sm-ethylenediaminetetramethylenephosphonate (EDTMP) in the treatment of patients with painful bone metastases. Eur J Cancer 33 (10): 1583-91, 1997. [PUBMED Abstract]
- Parker C, Nilsson S, Heinrich D, et al.: Alpha emitter radium-223 and survival in metastatic prostate cancer. N Engl J Med 369 (3): 213-23, 2013. [PUBMED Abstract]
- Bloch R: Rehabilitation medicine approach to cancer pain. Cancer Invest 22 (6): 944-8, 2004. [PUBMED Abstract]
- Richardson MA, Sanders T, Palmer JL, et al.: Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol 18 (13): 2505-14, 2000. [PUBMED Abstract]
- Bardia A, Barton DL, Prokop LJ, et al.: Efficacy of complementary and alternative medicine therapies in relieving cancer pain: a systematic review. J Clin Oncol 24 (34): 5457-64, 2006. [PUBMED Abstract]
General Approaches to Pain Treatment
Decision-Making Approach
Pain management varies widely in complexity. The decision-making process involves a careful consideration of many patient-related and pain-related factors. These may include, but are not limited to the following:
- Pain mechanism.
- Pain expression.
- Previous treatments.
- Available options.
- Prognosis.
Recognition of specific pain syndromes can be useful in guiding management.
Approach to Somatic Pain
Damage and/or inflammation involving the muscles, skin, joints, connective tissue, or bones can lead to activation of the nociceptive pathways that result in somatic pain. This type of pain is often well localized; may be described as sharp, achy, throbbing, and/or stabbing in nature; and often worsens with movement. It can often be managed with acetaminophen, anti-inflammatories, and opioids. Bone pain related to metastases is particularly common in cancer patients and is discussed below in more detail.
Bone pain
Bone pain due to metastatic disease is one of the most common causes of pain in cancer patients.[1,2] Bone is highly innervated tissue with receptors sensitive to mechanical damage.[3] The entrapment of nerve fibers in the collapsing bony matrix caused by increased osteoclastic activity and the release of inflammatory cytokines by cancer cells and immune cells are also central to the pathophysiology of bone pain.[3] Patients typically describe the pain as continuous, deep, and throbbing, with brief episodes of more-severe pain often precipitated by movement (i.e., a type of incident pain).
Most patients will require morphine or an equivalent opioid for adequate pain relief, although incident pain is less responsive. Adjunctive agents such as nonsteroidal anti-inflammatory drugs and corticosteroids are often prescribed and appear moderately effective and safe.[4]
In addition to providing analgesia, the clinician introduces treatments designed to prevent further weakening of skeletal integrity, which may lead to loss of functional status or further pain. Bone-targeting agents such as the bisphosphonates (zoledronic acid or pamidronate) or denosumab have been shown to reduce future skeletal-related events and to reduce the likelihood of increased pain or increased use of opioids in patients with advanced cancer.[5] For more information, see the Bisphosphonates and denosumab section.
Palliative radiation therapy produces complete or partial pain relief in up to 80% of treated patients; the median duration of relief exceeds 6 months.[6] For more information, see the External-Beam Radiation Therapy section.
Finally, orthopedic consultation is frequently necessary to determine whether operative intervention is required to prevent and/or treat pathological fractures.
Approach to Visceral Pain
Visceral pain is a type of nociceptive pain that originates in nociceptors innervating visceral organs. Several features of visceral pain inform the therapeutic approach:
- Not all internal organs have nociceptors. Typically, the hollow viscera (stomach, bowel, bladder, and ureters) are innervated and respond to mechanical-, inflammation-, and chemical-induced damage. For example, sensations originating from the liver or spleen are typically caused by distension of the capsule.
- There is a limited correlation between the degree of visceral injury and the intensity of the perceived pain.[7]
- The source of visceral pain is often difficult to localize. Referred pain may be perceived as remote from the actual affected organ (e.g., shoulder pain with splenic injury).
- In the phenomenon of sensitization, the normal activity of an organ is perceived as painful, such as stomach inflammation causing hyperawareness or hyperalgesia-related peristalsis of the stomach.
Opioids remain the core treatment for severe or distressing visceral pain.[8] Also important are radiographic studies to look for underlying causes that may be amendable to other interventions (e.g., bowel obstruction).
Approach to Neuropathic Pain
Pain with features suggestive of neuropathic pain is common among patients with cancer and can have substantial negative consequences. One study of 1,051 patients with cancer found that 17% had neuropathic pain. These patients reported worse physical, cognitive, and social functioning than did those with nociceptive pain; were on more analgesic medications and higher doses of opioids; and had a worse performance status.[9] Neuropathic pain is considered less responsive to opioids. Multiple therapeutic options instead of or in addition to opioids have been studied. Most of these studies were conducted in patients with nonmalignant sources of neuropathic pain and may not be applicable to patients with cancer with different etiologies for their neuropathic pain.
Gabapentin can be used as monotherapy in the first-line setting for neuropathic pain or in combination therapy if opioids, tricyclic antidepressants (TCAs), or other agents do not provide adequate relief. Gabapentin improved analgesia when added to opioids for uncontrolled cancer-related neuropathic pain.[10,11] When gabapentin was used adjuvantly to an opioid regimen, improvement in pain control was seen within 4 to 8 days.[12] In an open-label trial of pregabalin compared with fentanyl in 120 cancer patients with “definite” neuropathic pain, patients on pregabalin were twice as likely (73.3%) than those on fentanyl (36.7%) to report 30% or more reduction in pain, as measured by a visual analog scale (VAS).[13] Compared with monotherapy with amitriptyline, gabapentin, or placebo, pregabalin use resulted in a significant decrease in pain score when studied in neuropathic cancer pain.[14] In a randomized clinical trial of patients with head and neck cancer who were undergoing radiation therapy, pregabalin was shown to improve radiation therapy–related neuropathic pain, mood, and quality of life (QOL), with good tolerability.[15]
Notably, in a systemic review of neuropathic pain that included mostly patients with a nonmalignant source of neuropathic pain, the effect of gabapentin and pregabalin appeared less robust.[16] Data comparing gabapentin or pregabalin directly with TCAs and serotonin–norepinephrine reuptake inhibitors (SNRIs) are limited, especially in patients with cancer. Efficacy of TCAs and SNRIs appears to be comparable and, in some cases, superior to gabapentin or pregabalin. For more information, see the Chemotherapy-induced peripheral neuropathy (CIPN) section. Because of concerns about side effects and drug-drug interactions, many practitioners tend to start with gabapentin or pregabalin as first-line treatment for neuropathic pain. However, as noted below, certain neuropathic syndromes may be less responsive to these agents. For more information, see the sections on Postthoracotomy pain syndrome and Chemotherapy-induced peripheral neuropathy (CIPN). Studies have also examined the use of lidocaine patches, tramadol, topically applied capsaicin, and botulinum toxin A for use in patients with neuropathic pain [16] with inconclusive results.
Postmastectomy pain syndrome
Rates of postmastectomy pain range between 25% and 33%,[17–20] making this a common complication. Women with postmastectomy pain note more role limitations due to physical, emotional, and mental health issues.[17] Associations of postmastectomy pain with extent of surgery, radiation therapy, and chemotherapy are inconsistent across studies. One cross-sectional study found associations between postmastectomy pain and psychosocial factors such as depression, anxiety, somatization, and catastrophizing.[18,20]
A number of small studies have examined the effect of an anesthetic administered intraoperatively or immediately postoperatively, with varying results;[21] one group found a decrease in pain during the infusion but no benefits after the infusion until 12 months.[22,23] The use of venlafaxine or gabapentin for 10 days [24] or pregabalin for 7 days [25] starting 1 day before surgery may decrease postmastectomy pain, but confirmatory studies are needed.
Postthoracotomy pain syndrome
Defined as pain occurring 2 months after thoracotomy, postthoracotomy pain syndrome occurs in approximately 50% of patients and may be underreported and undertreated. The pain is thought to be related to damage to the intercostal nerve during surgery and from postoperative drainage via chest tubes. The pain includes both neuropathic and nonneuropathic components.[26]
Opioid and nonopioid analgesics are part of the standard approach to treatment. Several approaches in the immediate postoperative period are being investigated. An open-label noncontrolled study of 5% lidocaine patches showed improvement in pain scores 1 month postoperatively.[27] A small randomized trial of transcutaneous electrical nerve stimulation demonstrated decreased pain and reduced use of morphine and nonopioid analgesia in the immediate postoperative period.[28] Patients randomly assigned to receive intraoperative cryoanalgesia versus placebo were found to have less pain at time points up to 60 days postoperatively and reduced analgesic use in the first 3 days.[29] Further work is needed to confirm these results. In a randomized, double-blinded, placebo-controlled study of gabapentin started preoperatively and titrated over 5 days postoperatively, gabapentin failed to show benefit.[30]
Chemotherapy-induced peripheral neuropathy (CIPN)
Overview
Peripheral neuropathy is a common toxic effect of chemotherapy and is predominantly a sensory neuropathy. Patients report numbness and tingling in a stocking-and-glove distribution. CIPN is most commonly associated with the following:[31]
- Platinum compounds (e.g., oxaliplatin, cisplatin, and carboplatin, in descending order of severity).
- Taxanes (e.g., paclitaxel, docetaxel, and cabazitaxel).
- Thalidomide.
- Proteasome inhibitor (e.g., bortezomib, carfilzomib, and ixazomib).
- Vinca alkaloids.
Other agents, including ixabepilone, lenalidomide, and pomalidomide, are common sources of CIPN. With any of these agents, CIPN may limit the dose of chemotherapy delivered, which may affect the outcomes of treatment.[31] In one series of women treated with docetaxel, approximately one in four reported CIPN.[32] Although CIPN often improves after discontinuation or completion of chemotherapy, symptoms can linger for years for some patients, especially those treated with taxanes, with one study demonstrating a median 6.5-year duration of symptoms after diagnosis.[33,34] Newer immunotherapies, such as pembrolizumab and nivolumab, can produce peripheral neuropathies. The prevalence may become clear as more patients are treated with these agents.[35]
In two studies of women with breast cancer, peripheral neuropathy correlated negatively with QOL.[36][Level of evidence: II]; [37] The effect of a docetaxel regimen and patient characteristics on peripheral neuropathy and QOL was evaluated in a substudy of the NASBP B-30 trial.[37] The B-30 trial randomly assigned women with node-positive, early-stage breast cancer to one of three regimens: four cycles of doxorubicin plus cyclophosphamide every three weeks, followed by four cycles of docetaxel 100 mg/m2 (AC→T); four cycles of doxorubicin plus docetaxel 60 to 75 mg/m2; or four cycles of doxorubicin plus cyclophosphamide plus docetaxel 60 to 75 mg/m2. Overall, 41.9% of patients reported peripheral neuropathy 24 months after beginning treatment, with 10.3% reporting a severe symptom (“quite a bit”/“very much”/“bother” level). Treatment with AC→T, the regimen with the highest cumulative dose of docetaxel, resulted in increased severity of peripheral neuropathy compared with the other two regimens. Women who reported worse peripheral neuropathy symptoms had a statistically significant decreased QOL.
Preventing and reducing risk of CIPN
In 2020, the American Society of Clinical Oncology released a guideline update on the prevention and management of CIPN. At the time, there were no studies whose outcomes supported the recommendation of any neuropathy-preventive agents. A previously documented benefit of venlafaxine was refuted in a subsequent randomized, placebo-controlled, double-blind study, in which 50 patients were randomly assigned to receive venlafaxine extended-release 37.5 mg twice daily or a placebo. The study demonstrated no significant benefit for those who received venlafaxine.[38]
It is recommended that clinicians assess the risks and benefits of agents known to cause CIPN among patients with underlying neuropathy and with conditions that predispose to neuropathy. These conditions include the following:[39,40]
- Older age.
- Obesity.
- Lower physical activity.
- Diabetes.
- Longer planned duration of treatment.
- A family or personal history of hereditary peripheral neuropathy.
- Symptom burden.
- Alcohol intake.
The risk of long-term CIPN has also been documented. At 24 months after treatment initiation for early-stage breast cancer, women with the following characteristics were at an increased risk of continued peripheral neuropathy:[37]
- Preexisting peripheral neuropathy.
- Older age.
- Obesity.
- Mastectomy.
- Greater number of positive lymph nodes.
In a genome-wide association study, genetically determined African American ancestry was the most significant predictor of taxane-induced peripheral neuropathy.[41] It should be noted that the impact of risk-factor profiles may differ between racial and ethnic groups, as reported in one observational study of African American patients.[42] Eligible African American cancer survivors were surveyed to determine if there was an association between nongenetic risk factors and comorbidities with CIPN. Patients with CIPN were more likely to report hypertension, hypercholesterolemia, depression, diabetes, or increased body mass index (BMI). In contrast, alcohol consumption and tobacco use were not associated with increased risk of CIPN.
Treatment modalities for CIPN
Pharmacological treatments
American Society of Clinical Oncology (ASCO) guidelines [40,43] recommend against the use of many commonly prescribed agents for the treatment of existing CIPN. The exception is duloxetine because it is the only agent whose efficacy in treating CIPN is evidence based.[44] One large phase III trial identified an average decrease of 0.73 in the pain scores of patients who titrated up to 60 mg of duloxetine daily, when compared with placebo. Patients also had improvements in daily functioning and QOL.[44] Some argue that, while statistically significant, the difference of less than 1 (0.73) on a pain scale of 0 to 10 may not be clinically important.
Gabapentin failed to provide a benefit in CIPN when used as monotherapy in a randomized, double-blind, placebo-controlled trial.[44,45] The Cancer and Leukemia Group B prospective observational study evaluated 2,450 patients with stage III colon cancer. Increased severity of oxaliplatin-induced peripheral neuropathy (OIPN) may be linked to higher BMI, lower physical activity, diabetes mellitus, and a longer planned duration of treatment. Celecoxib and vitamin B6 intake did not attenuate OIPN.[46]
Evidence of the efficacy of nortriptyline and amitriptyline in CIPN is limited to small and frequently underpowered trials with mixed results.[47–49] Despite inconclusive trials, the authors suggested that a trial of TCAs, gabapentin, and topical baclofen/amitriptyline/ketamine may be reasonable in light of evidence supporting the benefit of these agents in other types of neuropathy and the relative lack of effective alternatives in this setting.[50]
Complementary and integrative therapies
Importantly, a large, randomized, multicenter, double-blind, placebo-controlled trial comparing the use of acetyl-L-carnitine with placebo in 409 women receiving taxane-based chemotherapy for breast cancer showed worsened CIPN. This worsening persisted over 2 years.[51]
Nonpharmacological treatments
Acupuncture
Studies of acupuncture for CIPN have been reported. For more information, see the Chemotherapy-induced peripheral neuropathy section in Acupuncture.
Scrambler therapy
Scrambler therapy is the application of electrical currents to discrete areas of the body as guided by the patient’s report of pain. The therapy is usually applied in ten consecutive sessions, although guidelines permit the skipping of weekend days. The technique is operator dependent, given the importance of identifying the area to treat and the application of the electrical current through five electrodes (referred to as artificial neurons). Furthermore, before daily scrambler therapy sessions, adjustments of the electrode placement and dose, titrated to pain relief, are required. Finally, it has been observed that misapplication of the currents induces worse pain.
The proposed mechanism of scrambler therapy begins with the observation that chronic pain may represent dysregulation of the somatosensory nervous system.[52] The application of the electrical currents activates surface receptors (synthetic pain) and provides an opportunity for the patient to reinterpret signals as nonpain. The proposed mechanism depends on patients decoding pain information as nonpainful.
There are two relevant randomized trials of scrambler therapy. One study randomly assigned 52 patients with CIPN to receive either standard guideline–consistent therapy (opioids, gabapentinoids, tricyclic antidepressants) or scrambler therapy.[53] The primary outcome was the mean VAS pain score at 1 month. The mean scores before treatment were 8.1 in the control group and 8.0 in the scrambler group. The mean scores in both groups decreased, but the improvement was greater for scrambler therapy: from 5.8 to 0.7 (P < .0001). The scores were maintained at 2 and 3 months. The lack of an effective sham control is a significant limitation, as is the potential that the attention paid to the patient may have a salutary effect.
A subsequent trial randomly assigned 50 patients to either scrambler therapy or a conventional transcutaneous electrical nerve stimulation (TENS) therapy.[54] The primary endpoint of the study was the proportion of patients who experienced a reduction of more than 50% in either pain or tingling at 2 weeks, compared to baseline. Fifty-six percent of patients who received scrambler therapy achieved the goal, compared with 28% of those who received TENS therapy. There was a corresponding improvement in Global Impression of Change scores for neuropathy symptoms. Patients in the scrambler therapy arm were more likely to recommend the therapy to friends. The choice of TENS therapy as a control is confounded by the lack of data related to its efficacy in treating CIPN.
Approach to Acute Procedural Pain
Bone marrow biopsy and aspiration
Bone marrow biopsy and aspiration cause pain in 84% of patients, with intensity reported as severe in 8% to 35%.[55] Factors associated with greater pain are the following:[56]
- Duration of the procedure (taking longer than 10 minutes).
- Younger age.
- Higher BMI.
- Female sex.
- Anxiety.
- Site of examination (sternum being the most painful).
- Inadequate information given before procedure.
- Lack of physician experience.
Pharmacological interventions for pain control vary from local anesthesia,[57] to intravenous sedation with benzodiazepines and/or opioids,[58] to the use of inhaled nitrous oxide,[59] to premedication with opioids. Addressing anxiety is an important nonpharmacological intervention.[56]
Lumbar puncture
Lumbar puncture is a diagnostic and staging tool for hematologic malignancies and solid tumors involving the central nervous system. Patients can develop post–lumbar puncture headache. Headaches usually develop hours to days after the procedure and are caused by leakage of cerebrospinal fluid, possible compensatory intracranial vessel dilatation, or increased tension on brain and meninges.[60] The use of an atraumatic small-bore needle has been found to reduce to incidence of post–lumbar puncture headaches.[61,62] A Cochrane review that included 13 small randomized trials mostly in noncancer patients reported some evidence to support the use of caffeine, gabapentin, hydrocortisone, and theophylline to treat post–lumbar puncture headache, and a lack of efficacy for sumatriptan, adrenocorticotropic hormone, pregabalin, and cosyntropin.[63]
Treatment of Pain in Specific Patient Populations
Geriatric cancer patients
Geriatric patients are defined as persons aged 65 years or older, with a significant increase in incidence of comorbidity after age 75 years.[64,65] Up to 80% of geriatric cancer patients have pain over the course of their disease.[66] There are unique concerns in the treatment of cancer pain in this patient population, resulting from a narrowed therapeutic index of many analgesic and adjunctive medications. Age-related physiologic changes alter pharmacodynamics and pharmacokinetic drug properties (see Table 7).[67–70] Increased comorbidities and the resulting polypharmacy put patients at risk of drug-disease and drug-drug interactions. In addition, few clinical trials have been performed in patients older than 65 years to confirm drug safety and efficacy. For geriatric patients, analgesic medications need to be started at low doses and titrated up gradually. The rationales behind this approach include higher pain thresholds,[71] differences in pain expression,[72] and greater effects on physical and psychosocial function in this patient population.[73] For more information, see the Pain Assessment section.
| Age-Related Physiological Change | Example of Affected Drugs |
|---|---|
| NSAID = nonsteroidal anti-inflammatory drug. | |
| aAdapted from American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons,[67] Miller,[68] Bosilkovska et al.,[69] and Lexicomp Online.[70] | |
| Decreased renal function | Increased accumulation of morphine metabolites |
| Increased risk of NSAID-induced renal dysfunction | |
| Increased body fat/decreased body water | Delayed elimination of lipophilic drugs such as methadone |
| Cachexia | Decreased fentanyl absorption from transdermal fentanyl patches [74] |
| Decreased hepatic function | Results in increased oral bioavailability and half-life of opioids |
| – Decrease dose: hydromorphone, oxycodone | |
| – Increase dose interval: morphine, oxycodone | |
| Reduced protein binding | Increased drug sensitivity/side effects |
| Reduced cytochrome P450 enzyme activity | Increased drug concentrations of fentanyl and methadone |
| Decreased gastrointestinal motility | Increased risk of opioid-induced constipation |
Geriatric patients are also at risk of undertreatment because of underreported pain, difficulty communicating, and physician concerns about adverse effects and aberrant behavior. Persistent, inadequately controlled pain leads to poor outcomes in older patients, including the following:[67]
- Functional impairment.
- Slower rehabilitation.
- Sleep and appetite changes.
- Increased use of health care resources.
Treatment of an underlying depression can help facilitate pain treatment.[75]
The American Geriatrics Society (AGS) recommends the use of acetaminophen over nonsteroidal anti-inflammatory drugs (NSAIDs), when possible, for the treatment of mild to moderate musculoskeletal pain.[67] Compared with acetaminophen, NSAIDs carry an increased risk of gastrointestinal bleed/peptic ulcer disease, kidney dysfunction, and exacerbation of hypertension, and heart failure. The maximum recommended dose of acetaminophen is 3 g per day, or 2 g if patients have comorbidities predisposing them to hepatoxicity. When the use of NSAIDs is necessary, as in cases of chronic inflammatory pain, particular caution should be used in patients with reduced renal function, gastropathy, cardiovascular disease, or dehydration.
Strategies to prevent gastrointestinal adverse effects include the following:[67]
- Co-administration of a gastroprotective agent such as an H2 receptor antagonist or a proton pump inhibitor.
- Use of a COX-2–selective NSAID.
- Use of a topical NSAID.
Opioids continue to be the mainstay of treating moderate to severe pain in geriatric patients. Older patients may be more sensitive to opioids because of the decreased renal and hepatic clearance of these drugs and their metabolites.[76,77] Geriatric patients may also need lower doses because they achieve greater analgesia from opioids. One retrospective study of opioid consumption in geriatric patients found that they need less opioid with acute and chronic pain therapy; they require less opioid regardless of route of administration; and incidental pain and/or neuropathic pain did not confound the correlation between age and opioid consumption but was associated with higher doses of opioids.[78] Geriatric patients are more susceptible to opioid adverse effects such as sedation and constipation. Guidelines recommend starting with lower opioid doses and increasing time between doses, with frequent reassessment of pain control to prevent underdosing. Meperidine should be avoided because of a lack of efficacy and increased risk of adverse effects, including seizure.[67]
Adjunct agents are often used with opioids to improve pain control for geriatric patients. Many of these adjunct agents are listed in the AGS Beers Criteria for Potentially Inappropriate Medication Use in Older Adults, to be avoided or used with caution in geriatric patients because of their increased risk of adverse effects [64] (see Table 8). For example, because of their high rate of anticholinergic effects, sedation, and risk of syncope and falls, tricyclic antidepressants commonly used to treat neuropathic pain conditions should be avoided in geriatric patients. Suggested alternatives for the treatment of neuropathic pain include duloxetine, gabapentin, topical capsaicin, and the lidocaine patch.[79]
| Drug/Class | Example | Rationale |
|---|---|---|
| CNS = central nervous system; COX-2 = cyclooxygenase-2; NSAIDs = nonsteroidal anti-inflammatory drugs. | ||
| aAdapted from American Geriatrics Society 2015 Beers Criteria Update Expert Panel.[64] | ||
| Tricyclic antidepressants | Amitriptyline, clomipramine, imipramine | Anticholinergic effects, sedation, orthostatic hypotension |
| Meperidine | Decreased efficacy, potential neurotoxicity | |
| Non–COX-2–selective NSAIDs | Ibuprofen, diclofenac, naproxen | Gastrointestinal bleed risk, increased blood pressure, renal toxicity |
| Skeletal muscle relaxants | Cyclobenzaprine, metaxalone, methocarbamol | Anticholinergic effects, sedation, risk of fracture |
| CNS | Avoid/reduce dose in renal impairment: | CNS adverse effects |
| – Gabapentin | ||
| – Pregabalin | ||
| – Duloxetine | ||
References
- Grond S, Zech D, Diefenbach C, et al.: Assessment of cancer pain: a prospective evaluation in 2266 cancer patients referred to a pain service. Pain 64 (1): 107-14, 1996. [PUBMED Abstract]
- Coleman RE: Clinical features of metastatic bone disease and risk of skeletal morbidity. Clin Cancer Res 12 (20 Pt 2): 6243s-6249s, 2006. [PUBMED Abstract]
- Falk S, Dickenson AH: Pain and nociception: mechanisms of cancer-induced bone pain. J Clin Oncol 32 (16): 1647-54, 2014. [PUBMED Abstract]
- Nabal M, Librada S, Redondo MJ, et al.: The role of paracetamol and nonsteroidal anti-inflammatory drugs in addition to WHO Step III opioids in the control of pain in advanced cancer. A systematic review of the literature. Palliat Med 26 (4): 305-12, 2012. [PUBMED Abstract]
- Patrick DL, Cleeland CS, von Moos R, et al.: Pain outcomes in patients with bone metastases from advanced cancer: assessment and management with bone-targeting agents. Support Care Cancer 23 (4): 1157-68, 2015. [PUBMED Abstract]
- Falkmer U, Järhult J, Wersäll P, et al.: A systematic overview of radiation therapy effects in skeletal metastases. Acta Oncol 42 (5-6): 620-33, 2003. [PUBMED Abstract]
- Patrizi F, Freedman SD, Pascual-Leone A, et al.: Novel therapeutic approaches to the treatment of chronic abdominal visceral pain. ScientificWorldJournal 6: 472-90, 2006. [PUBMED Abstract]
- Sikandar S, Dickenson AH: Visceral pain: the ins and outs, the ups and downs. Curr Opin Support Palliat Care 6 (1): 17-26, 2012. [PUBMED Abstract]
- Rayment C, Hjermstad MJ, Aass N, et al.: Neuropathic cancer pain: prevalence, severity, analgesics and impact from the European Palliative Care Research Collaborative-Computerised Symptom Assessment study. Palliat Med 27 (8): 714-21, 2013. [PUBMED Abstract]
- Caraceni A, Zecca E, Bonezzi C, et al.: Gabapentin for neuropathic cancer pain: a randomized controlled trial from the Gabapentin Cancer Pain Study Group. J Clin Oncol 22 (14): 2909-17, 2004. [PUBMED Abstract]
- Keskinbora K, Pekel AF, Aydinli I: Gabapentin and an opioid combination versus opioid alone for the management of neuropathic cancer pain: a randomized open trial. J Pain Symptom Manage 34 (2): 183-9, 2007. [PUBMED Abstract]
- Bennett MI: Effectiveness of antiepileptic or antidepressant drugs when added to opioids for cancer pain: systematic review. Palliat Med 25 (5): 553-9, 2011. [PUBMED Abstract]
- Raptis E, Vadalouca A, Stavropoulou E, et al.: Pregabalin vs. opioids for the treatment of neuropathic cancer pain: a prospective, head-to-head, randomized, open-label study. Pain Pract 14 (1): 32-42, 2014. [PUBMED Abstract]
- Mishra S, Bhatnagar S, Goyal GN, et al.: A comparative efficacy of amitriptyline, gabapentin, and pregabalin in neuropathic cancer pain: a prospective randomized double-blind placebo-controlled study. Am J Hosp Palliat Care 29 (3): 177-82, 2012. [PUBMED Abstract]
- Jiang J, Li Y, Shen Q, et al.: Effect of Pregabalin on Radiotherapy-Related Neuropathic Pain in Patients With Head and Neck Cancer: A Randomized Controlled Trial. J Clin Oncol 37 (2): 135-143, 2019. [PUBMED Abstract]
- Finnerup NB, Attal N, Haroutounian S, et al.: Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 14 (2): 162-73, 2015. [PUBMED Abstract]
- Meijuan Y, Zhiyou P, Yuwen T, et al.: A retrospective study of postmastectomy pain syndrome: incidence, characteristics, risk factors, and influence on quality of life. ScientificWorldJournal 2013: 159732, 2013. [PUBMED Abstract]
- Belfer I, Schreiber KL, Shaffer JR, et al.: Persistent postmastectomy pain in breast cancer survivors: analysis of clinical, demographic, and psychosocial factors. J Pain 14 (10): 1185-95, 2013. [PUBMED Abstract]
- Schreiber KL, Kehlet H, Belfer I, et al.: Predicting, preventing and managing persistent pain after breast cancer surgery: the importance of psychosocial factors. Pain Manag 4 (6): 445-59, 2014. [PUBMED Abstract]
- Schreiber KL, Martel MO, Shnol H, et al.: Persistent pain in postmastectomy patients: comparison of psychophysical, medical, surgical, and psychosocial characteristics between patients with and without pain. Pain 154 (5): 660-8, 2013. [PUBMED Abstract]
- Couceiro TC, Lima LC, Burle LM, et al.: Intravenous lidocaine for postmastectomy pain treatment: randomized, blind, placebo controlled clinical trial. Braz J Anesthesiol 65 (3): 207-12, 2015 May-Jun. [PUBMED Abstract]
- Ilfeld BM, Madison SJ, Suresh PJ, et al.: Persistent postmastectomy pain and pain-related physical and emotional functioning with and without a continuous paravertebral nerve block: a prospective 1-year follow-up assessment of a randomized, triple-masked, placebo-controlled study. Ann Surg Oncol 22 (6): 2017-25, 2015. [PUBMED Abstract]
- Ilfeld BM, Madison SJ, Suresh PJ, et al.: Treatment of postmastectomy pain with ambulatory continuous paravertebral nerve blocks: a randomized, triple-masked, placebo-controlled study. Reg Anesth Pain Med 39 (2): 89-96, 2014 Mar-Apr. [PUBMED Abstract]
- Amr YM, Yousef AA: Evaluation of efficacy of the perioperative administration of Venlafaxine or gabapentin on acute and chronic postmastectomy pain. Clin J Pain 26 (5): 381-5, 2010. [PUBMED Abstract]
- Reyad RM, Omran AF, Abbas DN, et al.: The Possible Preventive Role of Pregabalin in Postmastectomy Pain Syndrome: A Double-Blinded Randomized Controlled Trial. J Pain Symptom Manage 57 (1): 1-9, 2019. [PUBMED Abstract]
- Hopkins KG, Rosenzweig M: Post-thoracotomy pain syndrome: assessment and intervention. Clin J Oncol Nurs 16 (4): 365-70, 2012. [PUBMED Abstract]
- Garzón-Rodríguez C, Casals Merchan M, Calsina-Berna A, et al.: Lidocaine 5 % patches as an effective short-term co-analgesic in cancer pain. Preliminary results. Support Care Cancer 21 (11): 3153-8, 2013. [PUBMED Abstract]
- Fiorelli A, Morgillo F, Milione R, et al.: Control of post-thoracotomy pain by transcutaneous electrical nerve stimulation: effect on serum cytokine levels, visual analogue scale, pulmonary function and medication. Eur J Cardiothorac Surg 41 (4): 861-8; discussion 868, 2012. [PUBMED Abstract]
- Sepsas E, Misthos P, Anagnostopulu M, et al.: The role of intercostal cryoanalgesia in post-thoracotomy analgesia. Interact Cardiovasc Thorac Surg 16 (6): 814-8, 2013. [PUBMED Abstract]
- Grosen K, Drewes AM, Højsgaard A, et al.: Perioperative gabapentin for the prevention of persistent pain after thoracotomy: a randomized controlled trial. Eur J Cardiothorac Surg 46 (1): 76-85, 2014. [PUBMED Abstract]
- Cavaletti G, Alberti P, Frigeni B, et al.: Chemotherapy-induced neuropathy. Curr Treat Options Neurol 13 (2): 180-90, 2011. [PUBMED Abstract]
- Eckhoff L, Knoop A, Jensen MB, et al.: Persistence of docetaxel-induced neuropathy and impact on quality of life among breast cancer survivors. Eur J Cancer 51 (3): 292-300, 2015. [PUBMED Abstract]
- Kamgar M, Greenwald MK, Assad H, et al.: Prevalence and predictors of peripheral neuropathy after breast cancer treatment. Cancer Med 10 (19): 6666-6676, 2021. [PUBMED Abstract]
- Tanabe Y, Hashimoto K, Shimizu C, et al.: Paclitaxel-induced peripheral neuropathy in patients receiving adjuvant chemotherapy for breast cancer. Int J Clin Oncol 18 (1): 132-8, 2013. [PUBMED Abstract]
- Möhn N, Beutel G, Gutzmer R, et al.: Neurological Immune Related Adverse Events Associated with Nivolumab, Ipilimumab, and Pembrolizumab Therapy-Review of the Literature and Future Outlook. J Clin Med 8 (11): , 2019. [PUBMED Abstract]
- Engvall K, Gréen H, Fredrikson M, et al.: Impact of persistent peripheral neuropathy on health-related quality of life among early-stage breast cancer survivors: a population-based cross-sectional study. Breast Cancer Res Treat 195 (3): 379-391, 2022. [PUBMED Abstract]
- Bandos H, Melnikow J, Rivera DR, et al.: Long-term Peripheral Neuropathy in Breast Cancer Patients Treated With Adjuvant Chemotherapy: NRG Oncology/NSABP B-30. J Natl Cancer Inst 110 (2): , 2018. [PUBMED Abstract]
- Zimmerman C, Atherton PJ, Pachman D, et al.: MC11C4: a pilot randomized, placebo-controlled, double-blind study of venlafaxine to prevent oxaliplatin-induced neuropathy. Support Care Cancer 24 (3): 1071-8, 2016. [PUBMED Abstract]
- Molassiotis A, Cheng HL, Leung KT, et al.: Risk factors for chemotherapy-induced peripheral neuropathy in patients receiving taxane- and platinum-based chemotherapy. Brain Behav 9 (6): e01312, 2019. [PUBMED Abstract]
- Loprinzi CL, Lacchetti C, Bleeker J, et al.: Prevention and Management of Chemotherapy-Induced Peripheral Neuropathy in Survivors of Adult Cancers: ASCO Guideline Update. J Clin Oncol 38 (28): 3325-3348, 2020. [PUBMED Abstract]
- Schneider BP, Li L, Radovich M, et al.: Genome-Wide Association Studies for Taxane-Induced Peripheral Neuropathy in ECOG-5103 and ECOG-1199. Clin Cancer Res 21 (22): 5082-5091, 2015. [PUBMED Abstract]
- Trendowski MR, Lusk CM, Ruterbusch JJ, et al.: Chemotherapy-induced peripheral neuropathy in African American cancer survivors: Risk factors and quality of life outcomes. Cancer Med 10 (22): 8151-8161, 2021. [PUBMED Abstract]
- Hershman DL, Lacchetti C, Dworkin RH, et al.: Prevention and management of chemotherapy-induced peripheral neuropathy in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 32 (18): 1941-67, 2014. [PUBMED Abstract]
- Smith EM, Pang H, Cirrincione C, et al.: Effect of duloxetine on pain, function, and quality of life among patients with chemotherapy-induced painful peripheral neuropathy: a randomized clinical trial. JAMA 309 (13): 1359-67, 2013. [PUBMED Abstract]
- Rao RD, Michalak JC, Sloan JA, et al.: Efficacy of gabapentin in the management of chemotherapy-induced peripheral neuropathy: a phase 3 randomized, double-blind, placebo-controlled, crossover trial (N00C3). Cancer 110 (9): 2110-8, 2007. [PUBMED Abstract]
- Lee S, Ma C, Shi Q, et al.: Potential Mediators of Oxaliplatin-Induced Peripheral Neuropathy From Adjuvant Therapy in Stage III Colon Cancer: Findings From CALGB (Alliance)/SWOG 80702. J Clin Oncol 41 (5): 1079-1091, 2023. [PUBMED Abstract]
- Hammack JE, Michalak JC, Loprinzi CL, et al.: Phase III evaluation of nortriptyline for alleviation of symptoms of cis-platinum-induced peripheral neuropathy. Pain 98 (1-2): 195-203, 2002. [PUBMED Abstract]
- Kautio AL, Haanpää M, Saarto T, et al.: Amitriptyline in the treatment of chemotherapy-induced neuropathic symptoms. J Pain Symptom Manage 35 (1): 31-9, 2008. [PUBMED Abstract]
- Kalso E, Tasmuth T, Neuvonen PJ: Amitriptyline effectively relieves neuropathic pain following treatment of breast cancer. Pain 64 (2): 293-302, 1996. [PUBMED Abstract]
- Barton DL, Wos EJ, Qin R, et al.: A double-blind, placebo-controlled trial of a topical treatment for chemotherapy-induced peripheral neuropathy: NCCTG trial N06CA. Support Care Cancer 19 (6): 833-41, 2011. [PUBMED Abstract]
- Hershman DL, Unger JM, Crew KD, et al.: Two-Year Trends of Taxane-Induced Neuropathy in Women Enrolled in a Randomized Trial of Acetyl-L-Carnitine (SWOG S0715). J Natl Cancer Inst 110 (6): 669-676, 2018. [PUBMED Abstract]
- Marineo G: Inside the Scrambler Therapy, a Noninvasive Treatment of Chronic Neuropathic and Cancer Pain: From the Gate Control Theory to the Active Principle of Information. Integr Cancer Ther 18: 1534735419845143, 2019 Jan-Dec. [PUBMED Abstract]
- Marineo G, Iorno V, Gandini C, et al.: Scrambler therapy may relieve chronic neuropathic pain more effectively than guideline-based drug management: results of a pilot, randomized, controlled trial. J Pain Symptom Manage 43 (1): 87-95, 2012. [PUBMED Abstract]
- Loprinzi C, Le-Rademacher JG, Majithia N, et al.: Scrambler therapy for chemotherapy neuropathy: a randomized phase II pilot trial. Support Care Cancer 28 (3): 1183-1197, 2020. [PUBMED Abstract]
- Vanhelleputte P, Nijs K, Delforge M, et al.: Pain during bone marrow aspiration: prevalence and prevention. J Pain Symptom Manage 26 (3): 860-6, 2003. [PUBMED Abstract]
- Hjortholm N, Jaddini E, Hałaburda K, et al.: Strategies of pain reduction during the bone marrow biopsy. Ann Hematol 92 (2): 145-9, 2013. [PUBMED Abstract]
- Kuivalainen AM, Niemi-Murola L, Widenius T, et al.: Comparison of articaine and lidocaine for infiltration anaesthesia in patients undergoing bone marrow aspiration and biopsy. Eur J Pain 14 (2): 160-3, 2010. [PUBMED Abstract]
- Mainwaring CJ, Wong C, Lush RJ, et al.: The role of midazolam-induced sedation in bone marrow aspiration/trephine biopsies. Clin Lab Haematol 18 (4): 285-8, 1996. [PUBMED Abstract]
- Steedman B, Watson J, Ali S, et al.: Inhaled nitrous oxide (Entonox) as a short acting sedative during bone marrow examination. Clin Lab Haematol 28 (5): 321-4, 2006. [PUBMED Abstract]
- Vilming ST, Kloster R: The time course of post-lumbar puncture headache. Cephalalgia 18 (2): 97-100, 1998. [PUBMED Abstract]
- Yu LM, Chen DX, Zhou QX, et al.: Effects of histamine on immunophenotype and notch signaling in human HL-60 leukemia cells. Exp Biol Med (Maywood) 231 (10): 1633-7, 2006. [PUBMED Abstract]
- Strupp M, Schueler O, Straube A, et al.: “Atraumatic” Sprotte needle reduces the incidence of post-lumbar puncture headaches. Neurology 57 (12): 2310-2, 2001. [PUBMED Abstract]
- Basurto Ona X, Osorio D, Bonfill Cosp X: Drug therapy for treating post-dural puncture headache. Cochrane Database Syst Rev 7: CD007887, 2015.
- By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel: American Geriatrics Society 2015 Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 63 (11): 2227-46, 2015. [PUBMED Abstract]
- Piccirillo JF, Vlahiotis A, Barrett LB, et al.: The changing prevalence of comorbidity across the age spectrum. Crit Rev Oncol Hematol 67 (2): 124-32, 2008. [PUBMED Abstract]
- Rao A, Cohen HJ: Symptom management in the elderly cancer patient: fatigue, pain, and depression. J Natl Cancer Inst Monogr (32): 150-7, 2004. [PUBMED Abstract]
- American Geriatrics Society Panel on Pharmacological Management of Persistent Pain in Older Persons: Pharmacological management of persistent pain in older persons. J Am Geriatr Soc 57 (8): 1331-46, 2009. [PUBMED Abstract]
- Miller RA: Biology of aging and longevity. In: Halter JB, Ouslander JG, Tinetti ME, et al., eds.: Hazzard’s Geriatric Medicine and Gerontology. The McGraw-Hill Companies, Inc., 2009, pp 3-14.
- Bosilkovska M, Walder B, Besson M, et al.: Analgesics in patients with hepatic impairment: pharmacology and clinical implications. Drugs 72 (12): 1645-69, 2012. [PUBMED Abstract]
- Lexicomp Online. Hudson, Ohio: Lexi-Comp, Inc., 2021. Available online with subscription. Last accessed Feb. 9, 2024.
- Gagliese L, Melzack R: Age differences in nociception and pain behaviours in the rat. Neurosci Biobehav Rev 24 (8): 843-54, 2000. [PUBMED Abstract]
- McMillan SC: The relationship between age and intensity of cancer-related symptoms. Oncol Nurs Forum 16 (2): 237-41, 1989 Mar-Apr. [PUBMED Abstract]
- Sorkin BA, Rudy TE, Hanlon RB, et al.: Chronic pain in old and young patients: differences appear less important than similarities. J Gerontol 45 (2): P64-8, 1990. [PUBMED Abstract]
- Heiskanen T, Mätzke S, Haakana S, et al.: Transdermal fentanyl in cachectic cancer patients. Pain 144 (1-2): 218-22, 2009. [PUBMED Abstract]
- Gloth FM: Pain management in older adults: prevention and treatment. J Am Geriatr Soc 49 (2): 188-99, 2001. [PUBMED Abstract]
- McQuay HJ, Carroll D, Faura CC, et al.: Oral morphine in cancer pain: influences on morphine and metabolite concentration. Clin Pharmacol Ther 48 (3): 236-44, 1990. [PUBMED Abstract]
- Kaiko RF, Wallenstein SL, Rogers AG, et al.: Narcotics in the elderly. Med Clin North Am 66 (5): 1079-89, 1982. [PUBMED Abstract]
- Viganó A, Bruera E, Suarez-Almazor ME: Age, pain intensity, and opioid dose in patients with advanced cancer. Cancer 83 (6): 1244-50, 1998. [PUBMED Abstract]
- Hanlon JT, Semla TP, Schmader KE: Alternative Medications for Medications in the Use of High-Risk Medications in the Elderly and Potentially Harmful Drug-Disease Interactions in the Elderly Quality Measures. J Am Geriatr Soc 63 (12): e8-e18, 2015. [PUBMED Abstract]
Latest Updates to This Summary (02/12/2024)
The PDQ cancer information summaries are reviewed regularly and updated as new information becomes available. This section describes the latest changes made to this summary as of the date above.
Pharmacological Therapies for Pain Control
Added text about a cross-sectional study, which showed that analgesic medications taken at longer dose intervals were associated with increased adherence, adjusting for pain, symptom, demographic, and setting variables in the model (cited Stapleton et al. as reference 16).
This summary is written and maintained by the PDQ Supportive and Palliative Care Editorial Board, which is editorially independent of NCI. The summary reflects an independent review of the literature and does not represent a policy statement of NCI or NIH. More information about summary policies and the role of the PDQ Editorial Boards in maintaining the PDQ summaries can be found on the About This PDQ Summary and PDQ® Cancer Information for Health Professionals pages.
About This PDQ Summary
Purpose of This Summary
This PDQ cancer information summary for health professionals provides comprehensive, peer-reviewed, evidence-based information about the pathophysiology and treatment of pain. It is intended as a resource to inform and assist clinicians in the care of their patients. It does not provide formal guidelines or recommendations for making health care decisions.
Reviewers and Updates
This summary is reviewed regularly and updated as necessary by the PDQ Supportive and Palliative Care Editorial Board, which is editorially independent of the National Cancer Institute (NCI). The summary reflects an independent review of the literature and does not represent a policy statement of NCI or the National Institutes of Health (NIH).
Board members review recently published articles each month to determine whether an article should:
- be discussed at a meeting,
- be cited with text, or
- replace or update an existing article that is already cited.
Changes to the summaries are made through a consensus process in which Board members evaluate the strength of the evidence in the published articles and determine how the article should be included in the summary.
The lead reviewers for Cancer Pain are:
- Kristina B. Newport, MD, FAAHPM, HMDC (Penn State Hershey Cancer Institute at Milton S. Hershey Medical Center)
- Megan Reimann, PharmD, BCOP (Total CME)
- Andrea Ruskin, MD (VA Connecticut Healthcare System)
- Amy Wachholtz, PhD, MDiv, MS, ABPP (University of Colorado)
Any comments or questions about the summary content should be submitted to Cancer.gov through the NCI website’s Email Us. Do not contact the individual Board Members with questions or comments about the summaries. Board members will not respond to individual inquiries.
Levels of Evidence
Some of the reference citations in this summary are accompanied by a level-of-evidence designation. These designations are intended to help readers assess the strength of the evidence supporting the use of specific interventions or approaches. The PDQ Supportive and Palliative Care Editorial Board uses a formal evidence ranking system in developing its level-of-evidence designations.
Permission to Use This Summary
PDQ is a registered trademark. Although the content of PDQ documents can be used freely as text, it cannot be identified as an NCI PDQ cancer information summary unless it is presented in its entirety and is regularly updated. However, an author would be permitted to write a sentence such as “NCI’s PDQ cancer information summary about breast cancer prevention states the risks succinctly: [include excerpt from the summary].”
The preferred citation for this PDQ summary is:
PDQ® Supportive and Palliative Care Editorial Board. PDQ Cancer Pain. Bethesda, MD: National Cancer Institute. Updated <MM/DD/YYYY>. Available at: /side-effects/pain/pain-hp-pdq. Accessed <MM/DD/YYYY>. [PMID: 26389387]
Images in this summary are used with permission of the author(s), artist, and/or publisher for use within the PDQ summaries only. Permission to use images outside the context of PDQ information must be obtained from the owner(s) and cannot be granted by the National Cancer Institute. Information about using the illustrations in this summary, along with many other cancer-related images, is available in Visuals Online, a collection of over 2,000 scientific images.
Disclaimer
The information in these summaries should not be used as a basis for insurance reimbursement determinations. More information on insurance coverage is available on Cancer.gov on the Managing Cancer Care page.
Contact Us
More information about contacting us or receiving help with the Cancer.gov website can be found on our Contact Us for Help page. Questions can also be submitted to Cancer.gov through the website’s Email Us.